Seizures
![]() March, 14th, 2025
March, 14th, 2025
Benefit Summary
Learn about this burst of electrical activity in the brain and what causes it. Find out what to do if you see someone having a seizure.
Overview
, Overview, ,
A seizure is a sudden burst of electrical activity in the brain. It can cause changes in behavior, movements, feelings and levels of consciousness. Epilepsy is defined as having two or more seizures at least 24 hours apart that don’t have a known cause. But epilepsy doesn’t cause all seizures.
There are many types of seizures. They have a range of symptoms and vary in how much they affect your daily life. Seizure types also vary by where they begin in the brain and how far they spread. Most seizures last from 30 seconds to two minutes. A seizure that lasts longer than five minutes is a medical emergency.
Seizures can happen after a stroke or a head injury. An infection such as meningitis or another illness also may be the cause. But often the cause is not known.
Medicine can manage most seizures, but they can have side effects. Work with your healthcare professional to balance seizure management and medicine side effects.
Symptoms
Symptoms vary based on the type of seizure. They also can range from mild to serious. Seizure symptoms may include:
- Short-lived confusion.
- A staring spell.
- Jerking movements of the arms and legs that can’t be stopped.
- Loss of consciousness or awareness.
- Changes in thinking or emotions. These may include fear, anxiety or a feeling of already having lived the moment, called deja vu.
Most seizures fall into one of two classes called focal or generalized. The classes are based on how and where the brain activity causing the seizure began. If health professionals don’t know how the seizures began, they may say the seizures are of unknown onset.
Focal seizures
Focal seizures result from electrical activity in one area of the brain. This type of seizure can happen with or without passing out, called losing consciousness.
-
Focal seizures with impaired awareness. These seizures involve a change or loss of consciousness or awareness that feels like being in a dream. During these types of seizures, people may seem awake. But they stare into space and don’t respond to anything around them.
They may repeat movements such as hand rubbing and mouth movements, repeat certain words, or walk in circles. They may not remember the seizure or even know that it happened.
-
Focal seizures without impaired awareness. These seizures may change emotions. They also may change how things look, smell, feel, taste or sound. But people having a focal seizure don’t pass out.
During these types of seizures, people may feel angry, joyful or sad. Some people have nausea or odd feelings that are hard to describe. These seizures may cause trouble speaking and jerking of a body part such as an arm or a leg. They also may cause sudden symptoms such as tingling, dizziness and seeing flashing lights.
Symptoms of focal seizures may seem like those of other conditions of the brain or nervous system. These other conditions include migraine, mental illness or a condition that affects how the brain manages sleep-wake cycles, called narcolepsy.
Generalized seizures
Seizures that appear to involve all areas of the brain from the time they start are called generalized seizures. Types of generalized seizures include:
-
Absence seizures. Absence seizures often happen in children. These seizures once were called petit mal seizures. People who have absence seizures most often stare into space or make slight body movements such as eye blinking or lip smacking. The seizures most often last for 5 to 10 seconds.
Absence seizures can happen up to hundreds of times a day. They can come in clusters. And they can cause a brief loss of awareness.
- Tonic seizures. Tonic seizures cause muscles to get stiff. These seizures most often affect muscles in the back, arms and legs. People who have these seizures may pass out and fall to the ground.
- Atonic seizures. Atonic seizures cause a sudden loss of muscle use, most often in the legs. They’re also called drop seizures. People having this type of seizure may collapse.
- Clonic seizures. Clonic seizures are linked with jerking muscle movements. These seizures usually affect the neck, face and arms on both sides of the body.
- Myoclonic seizures. Myoclonic seizures most often cause sudden brief jerks or twitches of the arms and legs. People who have these seizures don’t often pass out.
-
Tonic-clonic seizures. Tonic-clonic seizures are the most common type of generalized seizure. They once were called grand mal seizures. They can cause passing out, body stiffness and shaking. They sometimes cause people to urinate or to bite their tongues.
Tonic-clonic seizures last for several minutes. Tonic-clonic seizures may start as focal seizures that spread to involve most or all of the brain.
Seizure stages
Seizures can have a beginning phase, a middle phase and an end phase. These phases also are called prodrome, ictal and postictal.
-
Prodrome. This is the earliest warning that a seizure may happen. During the prodrome, people may have a hard-to-describe sense that a seizure may happen. They also may have changes in behavior. This can happen in the hours or even days before a seizure.
The prodrome stage may include an aura. The aura is the first symptom of a seizure. Symptoms during the aura may include the feeling that a person or place is familiar, called deja vu, or a feeling that a person or place is not familiar.
Or people may simply feel strange, feel fear or panic, or even have good feelings. Symptoms also may include smells, sounds, tastes, blurred vision or racing thoughts. Most often, auras are feelings that are hard to describe. The prodrome may include headache, numbness, tingling, nausea or dizziness.
Many people with seizures have a prodrome or aura. But some people do not.
- Ictal phase. The ictal phase lasts from the first symptom, including the aura, to the end of the seizure. Symptoms of the ictal phase depend on the type of seizure.
-
Postictal phase. This is the period after a seizure during recovery. The postictal stage can last minutes or hours. Some people recover quickly, while others take hours. The length of the postictal phase depends on the type of seizure and what part of the brain was affected.
During this phase, people may be slow to respond, have trouble with memory, and have trouble talking or writing. They may feel sleepy, confused, dizzy, sad, scared, anxious or frustrated. They also may have nausea, a headache or weakness. They may feel thirsty or urinate.
When to see a doctor
Seek medical help right away if you have a seizure or if you see someone have a seizure and any of the following happens:
- The seizure lasts more than five minutes.
- The person isn’t breathing after the seizure stops.
- A second seizure follows right away.
- The person has a high fever.
- The person’s body overheats, called heat exhaustion.
- The person is pregnant.
- The person has diabetes.
- The seizure causes an injury.
- The seizure happens in water.
The first time you have a seizure, see a healthcare professional.
Causes
Seizures are caused by changes in the way nerve cells in the brain communicate. Nerve cells in the brain create, send and receive electrical impulses. The nerve cells are called neurons. The impulses allow the cells to communicate. Anything that gets in way of the communication pathways can lead to a seizure. Gene changes cause some types of seizures.
Epilepsy is a common cause of seizures. But not everyone who has a seizure has epilepsy. Sometimes the following can cause seizures:
- A high fever. When fever causes a seizure, it’s called a febrile seizure.
- An infection of the brain. This may include meningitis or encephalitis.
- Serious illness. This includes serious illness with COVID-19.
- Lack of sleep.
- Low blood sodium. This can happen if you take medicine that makes you urinate.
- Certain medicines that treat pain or depression or help people stop smoking.
- A new, active brain injury, such as head trauma. It can cause bleeding in an area of the brain or a stroke.
- The use of drugs that are sold on the streets. This includes amphetamines and cocaine.
- Alcohol misuse. Seizures can happen from withdrawal from alcohol or from drinking too much alcohol.
Risk factors
The following increase the risk of having a seizure:
- Head or brain injuries.
- Cognitive issues.
- Stroke.
- Alzheimer’s disease.
- Brain tumors.
- Alcohol or illicit drug misuse.
- Family history of seizures.
Complications
Having a seizure can sometimes lead to complications that can cause danger for you or others. You might be at risk of:
- Falling. If you fall during a seizure, you can injure your head or break a bone.
- Drowning. If you have a seizure while swimming or bathing, you’re at risk of drowning.
- Car accidents. A seizure can cause loss of awareness or not being able to control a vehicle while driving.
- Pregnancy complications. Seizures during pregnancy pose dangers to pregnant people and their babies. And certain antiseizure medicines increase the risk of health conditions present at birth. If you have epilepsy and plan to become pregnant, work with your healthcare professional to check to see if your medicines need to be adjusted during pregnancy.
- Mental health conditions. People with seizures are more likely to have depression, anxiety or other mental health conditions. This can be from dealing with seizures or from the side effects of antiseizure medicines.
- Sudden, unexpected death. Rarely, a single seizure causes death. This is called sudden unexpected death in epilepsy (SUDEP). Seizures that aren’t managed well and other factors play a role in the risk of SUDEP. But experts don’t know the overall risks or the cause. Good treatment of seizures is vital in preventing SUDEP.
Prevention
People who have more than one seizure should stay away from things that can cause a seizure, such as:
- Not sleeping enough.
- Using alcohol or illicit drugs.
- Stress.
- Being around flashing lights.
Diagnosis
After a seizure, your healthcare professional reviews your symptoms and medical history and does a physical exam. You may have tests to find the cause of your seizure. Tests also may show how likely it is that you’ll have another seizure.
Tests may include:
- A neurological exam. This is to look at your behavior, motor abilities and how your brain works.
- Blood tests. A blood sample can show blood sugar levels and look for signs of infections or gene conditions. A health professional also may check the levels of salts in the body that manage the balance of fluids. These salts are called electrolytes.
- A spinal tap. This procedure collects a sample of fluid from the spine for testing. Also called a lumbar puncture, a spinal tap may show whether an infection caused a seizure.
-
An electroencephalogram (EEG). In this test, electrodes are put on the scalp to record the electrical activity of the brain. The electrical activity shows up as wavy lines on an EEG recording. The EEG may show a pattern that tells whether a seizure is likely to happen again.
EEG testing also may help rule out other conditions that have symptoms like those of epilepsy. This test may be done at a clinic, overnight at home or over a few nights in the hospital.
Imaging tests may include:
- MRI. An MRI scan uses powerful magnets and radio waves to create a detailed view of the brain. An MRI may show changes in the brain that could lead to seizures.
- CT scan. A CT scan uses X-rays to get cross-sectional images of the brain. CT scans can show changes in the brain that might cause a seizure. Those changes may include tumors, bleeding and cysts.
- Positron emission tomography (PET). A PET scan uses a small amount of low-dose radioactive material that’s put into a vein. The material helps show active areas of the brain and brain changes.
-
Single-photon emission computerized tomography (SPECT). A SPECT test uses a small amount of low-dose radioactive material that’s put into a vein. The test creates a detailed 3D map of the blood flow in the brain that happens during a seizure.
A healthcare professional also may do a type of SPECT test called subtraction ictal SPECT coregistered with MRI (SISCOM). The test may give results with even more detail. This test is usually done in a hospital with overnight EEG recording.

An EEG records the electrical activity of the brain through electrodes put on the scalp. EEG results show changes in brain activity. This may help diagnose brain conditions such as epilepsy and other seizure conditions.

During a high-density EEG test, a healthcare professional puts electrodes close together on the scalp. Like regular EEG, high-density EEG records brain activity. A high-density EEG test can help find the area in the brain where seizures happen.

A CT scan can show nearly all parts of the body. Healthcare professionals use it to diagnose disease or injury and to plan medical, surgical or radiation treatment.

These SPECT images show the blood flow in the brain when there’s no seizure activity (left) and during a seizure (middle). The subtraction SPECT coregistered to MRI (right) helps pinpoint the area of seizure activity by overlapping the SPECT results with brain MRI results.
Pinpointing seizure location Treatment
Not everyone who has one seizure has another one. So your healthcare professional may not start treatment unless you’ve had more than one.
The goal in seizure treatment is to find the best therapy that stops seizures with the fewest side effects.
Medications
Treatment of seizures often involves antiseizure medicines. There are many types of antiseizure medicine.
Finding the right medicine and dosage can be hard. Some people try several medicines before finding the right one in the right dosage. Common side effects may include weight changes, dizziness, tiredness and mood changes. Very rarely, more-serious side effects can cause damage to the liver or bone marrow.
A healthcare professional thinks about your condition, how often you have seizures, your age and other factors when choosing which medicine to prescribe. The health professional also reviews other medicines you take to make sure that the antiseizure medicines won’t interact with them.
Dietary therapy
Following a ketogenic diet can improve seizure management. A ketogenic diet is high in fat and very low in carbohydrates. But it can be hard to follow because there’s a small range of foods allowed.
Other versions of a high-fat, low-carbohydrate diet also may be helpful but not work as well. These diets include low glycemic index and Atkins diets. Experts are still studying these diets.
Surgery
If treatment with at least two antiseizure medicines doesn’t work, you might have surgery to stop the seizures. Surgery works best for people who have seizures that always begin in the same place in the brain. Types of surgery include:
- Lobectomy. Surgeons find and remove the area of the brain where seizures begin.
- Thermal ablation, also called laser interstitial thermal therapy. This less invasive procedure aims highly concentrated energy at a target in the brain where seizures begin. This destroys the brain cells that cause seizures.
- Multiple subpial transection. This type of surgery involves making several cuts in areas of the brain to prevent seizures. Surgeons do this most often when they can’t safely remove the area of the brain where seizures start.
- Corpus callosotomy. This surgery cuts the network of links between the neurons of the right and left halves of the brain. This is used to treat seizures that start in one half of the brain and travel to the other half. But even after surgery, seizures may still happen on the side of the brain where they started.
-
Hemispherotomy. This surgery separates one side of the brain from the rest of the brain and body. Surgeons use this type of surgery only when medicines don’t manage seizures and when seizures affect only half the brain.
This surgery can cause the loss of many daily functional abilities. But children often can get those abilities back with rehabilitation.
Electrical stimulation
If surgeons can’t remove or separate the area of the brain where seizures start, devices that provide electrical stimulation may help. They can work with antiseizure medicines to reduce seizures. Stimulation devices that may offer seizure relief include:
- Vagus nerve stimulation. A device placed under the skin of the chest stimulates the vagus nerve in the neck. This sends signals to the brain that lessens seizures.
- Responsive neurostimulation. Surgeons place this device on the brain or in brain tissue. The device can tell when seizure activity starts. It sends electrical stimulation to stop the seizure.
- Deep brain stimulation. Surgeons place thin wires called electrodes in certain areas of the brain to produce electrical impulses. The impulses help the body manage the brain activity that causes seizures. The electrodes attach to a pacemakerlike device placed under the skin of the chest. The device manages how much stimulation happens.
Pregnancy and seizures
People who’ve had seizures most often can have healthy pregnancies. But some medicines used to treat seizures sometimes can cause health conditions that are present at birth.
Valproic acid is a medicine for generalized seizures that has been linked with cognitive issues and neural tube defects, such as spina bifida, in babies. The American Academy of Neurology advises against using valproic acid during pregnancy because of risks to babies.
Talk with your healthcare professional about the risks of antiseizure medicines, including the risk of health conditions present at birth. Make a plan with your health professional before you get pregnant. Pregnancy can change medicine levels.
Some people may need to change the dosage of seizure medicine before or during pregnancy. The goal is to be on the lowest dose of the safest seizure medicine that manages seizures.
Taking folic acid before pregnancy may help prevent some complications related to taking antiseizure medicines while pregnant. Folic acid is in standard prenatal vitamins. Experts suggest that all people of childbearing age take folic acid while taking antiseizure medicines.
Birth control and antiseizure medicines
Some antiseizure medicines keep birth control from working as well. Check with your healthcare professional to see whether your medicine affects your birth control. You may need to try other forms of birth control.
Potential future treatments
Researchers study other therapies that might treat seizures. These include therapies to stimulate the brain without surgery.
One area of research showing promise is MRI-guided focused ultrasound. The therapy involves pointing ultrasound beams, which are sound waves, to an area of the brain that’s causing seizures. The beam creates energy to destroy brain tissue without surgery.
This type of therapy can reach deeper brain structures. It also can focus on a target without damaging the nearby tissue.

In vagus nerve stimulation, a device placed under the skin of the chest stimulates the vagus nerve in the neck. This sends signals to the brain that lessen seizures.
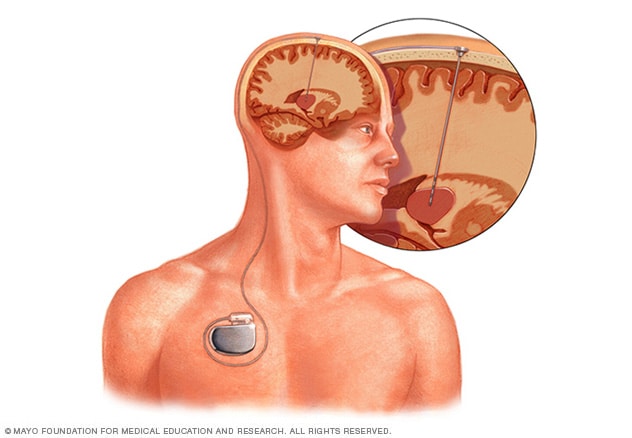
Deep brain stimulation involves putting an electrode deep within the brain. The amount of stimulation delivered by the electrode is controlled by a device placed under the skin in the chest. A wire that travels under the skin connects the device to the electrode.
Deep brain stimulation Lifestyle and home remedies
Here are some steps you can take to help manage seizures:
- Take medicine correctly. Don’t change the dose without first talking with your healthcare professional. If you think that your medicine needs a change, always talk with your health professional.
- Get enough sleep. Lack of sleep can trigger seizures. Be sure to get enough rest every night.
- Wear a medical alert bracelet. This will help emergency responders know how to treat you if you have a seizure.
- Be active. Exercising and being active may help keep you healthy and reduce depression. Make sure to drink enough water. And rest if you get tired during exercise.
- Make healthy life choices. Managing stress, limiting alcohol use and not smoking all are part of a healthy lifestyle.
Treatment
Personal safety
Seizures don’t often result in serious injury. But if you have repeated seizures, you might injure yourself. These steps can help you avoid injury during a seizure:
- Take care near water. Don’t swim alone or ride in a boat without someone nearby.
- Wear a helmet. Wear a helmet during activities such as bike riding or playing sports.
- Take showers. Don’t take baths unless someone is near you.
- Soften your home. Pad sharp corners, buy furniture with rounded edges and choose chairs that have arms to keep you from falling off. Think about having carpet with thick padding to protect you if you fall.
- Don’t work high up. And don’t use heavy machinery.
- Have a list of seizure first-aid tips. Put them in a place where people can see them. Include phone numbers people might need if you have a seizure.
-
Consider a seizure detection device. In the U.S., the Food and Drug Administration (FDA) has cleared a watchlike device that can tell when a tonic-clonic seizure is about to happen (EpiMonitor). The device alerts loved ones or caregivers so that they can check on you and make sure you’re safe.
Another FDA-approved device attaches to a muscle in the arm called the bicep to watch for seizure activity (Brain Sentinel SPEAC). Talk with your healthcare professional to see if using this type of device might be right for you.
Lifestyle and home remedies
Seizure first aid
It’s helpful to know what to do if you see someone having a seizure. If you’re at risk of having seizures, give this information to family, friends and co-workers. Then they’ll know what to do if you have a seizure.
To help someone during a seizure, take these steps:
- Carefully roll the person onto one side.
- Place something soft under the person’s head.
- Loosen tight neckwear.
- Don’t put your fingers or other objects in the person’s mouth.
- Don’t try to restrain the person.
- Clear away dangerous objects if the person is moving.
- Stay with the person until medical help arrives.
- Watch the person closely so that you can tell medical helpers what happened.
- Time the seizure.
- Stay calm.
Coping and support
Stress due to living with a seizure condition can affect your mental health. Talk with your healthcare professional about your feelings. Look for ways to find help.
At home
Your family members can provide support you may need. Tell them what you know about your seizures. Let them know they can ask you questions. Ask them about their worries. Help family members learn about your condition. Share materials or other resources that your healthcare professional gives you.
At work
Talk with your supervisor about your seizures and how they affect you. Discuss what you need your supervisor or co-workers to do if you have a seizure at work. Talk with your co-workers about seizures. This will help them understand and give you more support.
You’re not alone
Reach out to family and friends. Ask your healthcare professional about local support groups or join an online support community. Don’t be afraid to ask for help. Having a strong support system is vital to living with any medical condition.
Preparing for an appointment
Sometimes seizures need medical help right away. So there’s not always time to prepare for an appointment.
But you may see your primary healthcare professional or be sent to a specialist. You might see a specialist trained in brain and nervous system conditions, called a neurologist. Or you might see a neurologist trained in epilepsy, known as an epileptologist.
Here’s some information to help you get ready for your appointment.
What you can do
- Write down what you remember about the seizure. Include when and where it happened, symptoms you had and how long it lasted, if you know. Ask anyone who saw the seizure to help you fill in the details.
- Be aware of any restrictions before your appointment. When you make the appointment, ask if there’s anything you need to do ahead of time to be ready for medical tests or exams.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you take, including doses.
- Take a family member or friend to your appointment. Someone who’s with you can help you remember all the information you get. And the person who goes with you may be able to answer questions about your seizure that you can’t.
- Write down questions to ask your healthcare professional. Making a list of questions can help you make the most of your time during your visit.
For seizures, some basic questions to ask include:
- What do you think caused my seizure?
- What tests do I need?
- What treatment do you suggest?
- How likely is it that I might have another seizure?
- How can I make sure that I don’t hurt myself if I have another seizure?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Are there brochures or other printed material that I can have? What websites do you suggest?
Be sure to ask all the questions you have.
What to expect from your doctor
A healthcare professional is likely to ask you questions, such as:
- Can you describe your seizure episode?
- Was anyone there to see what happened?
- What did you feel just before the seizure? What about right after the seizure?
- Have you had a seizure or other neurological condition in the past?
- Do you have any family members who have been diagnosed with a seizure condition or epilepsy?
- Have you recently traveled outside the country?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



