Hypertrophic cardiomyopathy
![]() September, 24th, 2024
September, 24th, 2024
Benefit Summary
In this condition, the heart muscle thickens, which makes it harder for the heart to pump blood. Learn about the causes and treatment.
Overview
, Overview, ,
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle becomes thickened, also called hypertrophied. The thickened heart muscle can make it harder for the heart to pump blood.
Many people with hypertrophic cardiomyopathy don’t realize they have it. That’s because they have few, if any, symptoms. But in a small number of people with HCM, the thickened heart muscle can cause serious symptoms. These include shortness of breath and chest pain. Some people with HCM have changes in the heart’s electrical system. These changes can result in life-threatening irregular heartbeats or sudden death.
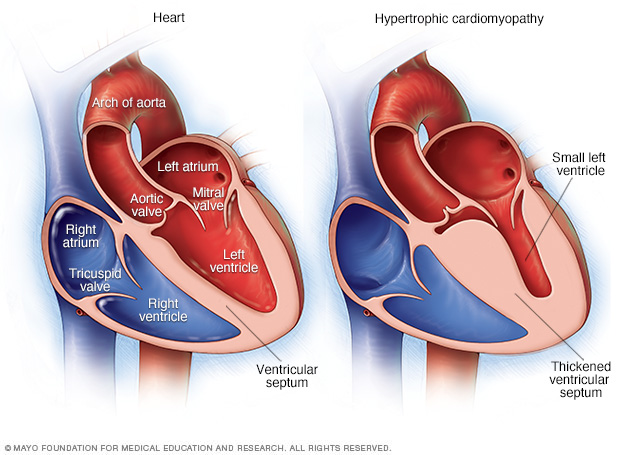
In hypertrophic cardiomyopathy, the muscular heart wall called the septum often becomes thicker than usual. But the thickening can happen anywhere in the left lower heart chamber, also called the left ventricle.
Hypertrophic cardiomyopathy Symptoms
Symptoms of hypertrophic cardiomyopathy can include one or more of the following:
- Chest pain, especially during exercise.
- Fainting, especially during or just after exercise or other physical activity.
- Sensation of fast, fluttering or pounding heartbeats called palpitations.
- Shortness of breath, especially during exercise.
When to see a doctor
Many conditions can cause shortness of breath and fast, pounding heartbeats. It’s important to get a prompt checkup to find the cause and receive the right care. See your healthcare professional if you have a family history of HCM or any symptoms related to hypertrophic cardiomyopathy.
Call 911 or your local emergency number if you have any of the following symptoms for more than a few minutes:
- Rapid or irregular heartbeat.
- Trouble breathing.
- Chest pain.
Causes
Hypertrophic cardiomyopathy usually is caused by changes in genes that cause the heart muscle to thicken.
Hypertrophic cardiomyopathy typically affects the wall between the two bottom chambers of the heart. This wall is called the septum. The chambers are called the ventricles. The thickened wall might block blood flow out of the heart. This is called obstructive hypertrophic cardiomyopathy.
If there’s no significant blocking of blood flow, the condition is called nonobstructive hypertrophic cardiomyopathy. But the heart’s main pumping chamber, called the left ventricle, might stiffen. This makes it hard for the heart to relax. The stiffness also lessens the amount of blood the ventricle can hold and send to the body with each heartbeat.
Heart muscle cells also become arranged differently in people with hypertrophic cardiomyopathy. This is called myofiber disarray. It can trigger irregular heartbeats in some people.
Risk factors
Hypertrophic cardiomyopathy usually is passed down through families. That means it’s inherited. People with one parent with hypertrophic cardiomyopathy have a 50% chance of having the gene change that causes the disease.
Parents, children, or brothers or sisters of a person with hypertrophic cardiomyopathy should ask their healthcare team about screening tests for the disease.
Complications
Complications of hypertrophic cardiomyopathy can include:
- Atrial fibrillation (AFib). A thickened heart muscle and changes in the structure of heart cells can trigger an irregular and often very rapid heartbeat called AFib. AFib also raises the risk of blood clots, which can travel to the brain and cause a stroke.
- Blocked blood flow. In many people, the thickened heart muscle blocks the blood flow leaving the heart. This can cause shortness of breath with activity, chest pain, dizziness and fainting spells.
- Mitral valve disease. If the thickened heart muscle blocks the blood flow leaving the heart, the valve between the left heart chambers might not close properly. That valve is called the mitral valve. If it doesn’t close properly, blood can leak backward into the left upper chamber. This is a condition called mitral valve regurgitation. It might make hypertrophic cardiomyopathy symptoms worse.
- Dilated cardiomyopathy. In a small number of people with HCM, the thickened heart muscle becomes weak and doesn’t work well. The condition tends to start in the left lower heart chamber. The chamber becomes larger. The heart pumps with less force.
- Heart failure. Over time, the thickened heart muscle can become too stiff to fill the heart with blood. As a result, the heart can’t pump enough blood to meet the body’s needs.
- Fainting, also called syncope. An irregular heartbeat or blockage of blood flow can sometimes cause fainting. Unexplained fainting can be related to sudden cardiac death, especially if it’s happened recently and in a young person.
- Sudden cardiac death. Rarely, hypertrophic cardiomyopathy can cause heart-related sudden death in people of all ages. Many people with hypertrophic cardiomyopathy don’t realize they have it. As a result, sudden cardiac death might be the first sign of the condition. It can happen in young people who seem healthy, including high school athletes and other young, active adults.
Prevention
There is no known way to prevent hypertrophic cardiomyopathy (HCM). It’s important to find the condition with tests as early as possible to guide treatment and prevent complications.
Hypertrophic cardiomyopathy usually is passed down in families. If you have a parent, brother, sister or child with hypertrophic cardiomyopathy, ask your healthcare team if genetic screening is right for you. But not everyone with HCM has a gene change that tests can detect. Also, some insurance companies may not cover genetic testing.
If genetic testing isn’t done, or if the results aren’t helpful, screening may be done with repeated echocardiograms. Echocardiograms use sound waves to make pictures of the heart.
For people who have a family member with hypertrophic cardiomyopathy:
- Echocardiogram screenings are recommended starting at about age 12.
- Screening with echocardiograms should continue every 1 to 3 years through ages 18 to 21.
- After that, the screenings can be done every five years through adulthood.
You may need to have an echocardiogram more often based on your overall health and healthcare team’s preference.
Diagnosis
A healthcare professional examines you and listens to your heart with a device called a stethoscope. A heart murmur may be heard while listening to the heart.
A member of your healthcare team usually asks questions about your symptoms and your medical and family history. Genetic testing or counseling may be recommended if you have a family history of the condition.
Tests
Tests are done to check the heart and look for causes of any symptoms.
- Echocardiogram. An echocardiogram often is used to diagnose hypertrophic cardiomyopathy. Sound waves are used to create images of the beating heart. This test shows how well the heart’s chambers and valves are pumping blood. An echocardiogram also can see if the heart’s muscle is thicker than it should be.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches called electrodes are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which prints or displays the test results. An ECG can show irregular heartbeats and signs of heart thickening.
- Holter monitor. This small, portable ECG device records the heart’s activity. It’s worn for a day or two while you do your regular activities.
- Cardiac MRI. This test uses powerful magnets and radio waves to create images of the heart. It provides information about the heart muscle and how the heart and heart valves work. This test often is done with an echocardiogram.
- Stress test. A stress test often involves walking on a treadmill or riding a stationary bike while the heart is monitored. Exercise stress tests help reveal how the heart responds to physical activity.
- Cardiac CT scan. Rarely, this test is done to diagnose hypertrophic cardiomyopathy. But it may be suggested if an MRI can’t be used. A cardiac CT scan uses X-rays to make pictures of the heart and chest. It can show the size of the heart.
Treatment
The goals of hypertrophic cardiomyopathy treatment are to ease symptoms and prevent sudden cardiac death in people at high risk. Treatment depends on how severe the symptoms are.
If you have cardiomyopathy and are pregnant or thinking about pregnancy, talk with your healthcare professional. You might be referred to a doctor with experience in high-risk pregnancies. This doctor might be a perinatologist or a maternal-fetal medicine specialist.
Medications
Medicines can help reduce how strongly the heart muscle squeezes and slow the heart rate. That way, the heart can pump blood better. Medicines to treat hypertrophic cardiomyopathy and its symptoms might include:
- Beta blockers such as metoprolol (Lopressor, Toprol-XL), propranolol (Inderal LA, Innopran XL) or atenolol (Tenormin).
- Calcium channel blockers such as verapamil (Verelan) or diltiazem (Cardizem, Tiazac, others).
- A medicine called mavacamten (Camzyos) that reduces the strain on the heart. It can treat obstructive HCM in adults with symptoms. Your healthcare team may suggest this medicine if you can’t take or don’t get better with beta blockers or verapamil.
- Heart rhythm medicines such as amiodarone (Pacerone) or disopyramide (Norpace).
- Blood thinners such as warfarin (Jantoven), dabigatran (Pradaxa), rivaroxaban (Xarelto) or apixaban (Eliquis). Blood thinners can help prevent blood clots if you have atrial fibrillation or the apical type of hypertrophic cardiomyopathy. Apical HCM can raise the risk of sudden cardiac death.
Surgeries or other procedures
Several surgeries or procedures are available to treat cardiomyopathy or its symptoms. They include:
-
Septal myectomy. This open-heart surgery might be recommended if medicines don’t improve symptoms. It involves removing part of the thickened, overgrown wall between the heart chambers. This wall is called the septum. Septal myectomy helps improve blood flow out of the heart. It also reduces backward flow of blood through the mitral valve.
The surgery can be done using different approaches, depending on the location of the thickened heart muscle. In one type, called apical myectomy, surgeons remove thickened heart muscle from near the tip of the heart. Sometimes the mitral valve is repaired at the same time.
- Septal ablation. This procedure use alcohol to shrink the thickened heart muscle. A long, thin tube called a catheter is placed into an artery that supplies blood to the affected area. Alcohol flows through the tube. Changes in the heart’s electrical signaling system, also called a heart block, is one complication. A heart block must be treated with a pacemaker. The small device is placed in the chest to help control the heartbeat.
- Implantable cardioverter-defibrillator (ICD). This device is placed under the skin near the collarbone. It continuously checks the heart rhythm. If the device finds an irregular heartbeat, it sends out low- or high-energy shocks to reset the heart’s rhythm. Use of an ICD has been shown to help prevent sudden cardiac death, which occurs in a small number of people with hypertrophic cardiomyopathy.
- Cardiac resynchronization therapy (CRT) device. Rarely, this implanted device is used as a treatment for hypertrophic cardiomyopathy. It can help the chambers of the heart squeeze in a way that’s more organized and efficient.
- Ventricular assist device (VAD). This implanted device also is rarely used to treat hypertrophic cardiomyopathy. It helps blood flow through the heart.
- Heart transplant. This is surgery to replace a diseased heart with a donor’s healthy heart. It can be a treatment option for end-stage heart failure when medicines and other treatments no longer work.
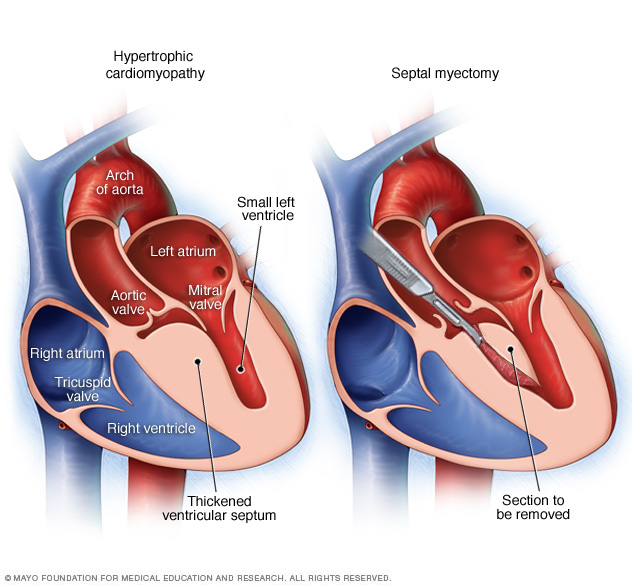
A septal myectomy is an open-heart surgery. A surgeon removes part of the thickened, overgrown septum between the lower heart chambers called the ventricles, as shown in the heart on the right.

An apical myectomy is an open-heart surgery to treat hypertrophic cardiomyopathy. A surgeon removes remove thickened heart muscle from near the tip of the heart.
Apical myectomy Lifestyle and home remedies
Lifestyle changes can lower the risk of complications related to hypertrophic cardiomyopathy. Try these healthy habits:
- Exercise. Ask your healthcare professional about the amount and type of exercise that’s safe for you.
- Eat a healthy diet. Eat a healthy diet that’s low in salt and solid fats and rich in fruits, vegetables and whole grains.
- Don’t smoke. If you smoke and can’t quit on your own, talk to a healthcare professional about strategies or programs to help.
- Stay at a healthy weight. This helps prevent excessive stress on the heart. It also lowers health risks linked with surgery or other procedures. Talk with your care team to set realistic goals for body mass index (BMI) and weight.
- Limit or stay away from alcohol. Sometimes, irregular heart rhythms and blocked blood flow are triggered or made worse by alcohol use. Ask your healthcare professional how much alcohol, if any, is safe for you to drink. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Control blood pressure and cholesterol. High blood pressure and high cholesterol increase the risk of heart disease. Make lifestyle changes and take medicines as directed to manage high blood pressure or high cholesterol. Get regular health checkups. Your healthcare professional might recommend regular follow-up appointments to check on your condition. Tell your care team if you have new or worsening symptoms.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to a healthcare professional about strategies that might help.
Coping and support
Connect with friends and family or a support group. You may find that talking about hypertrophic cardiomyopathy with others in similar situations can help.
It also is important to control emotional stress. Getting more exercise and practicing mindfulness are ways to ease stress. If you have anxiety or depression, talk to your healthcare team about strategies to help.
Preparing for an appointment
You may be referred to a doctor trained in heart diseases. This type of care professional is called a cardiologist. Here’s some information to help you prepare for your appointment.
What you can do
When you make the appointment, ask if you need to follow any restrictions before the checkup. For instance, you may need to change your activity level or your diet. Make a list of:
- Your symptoms and when they began.
- All medicines, vitamins and supplements you take, including doses.
- Key medical information, including other conditions you have and any family history of heart disease.
- Questions to ask your healthcare professional.
Questions to ask your healthcare professional might include:
- What’s the most likely cause of my symptoms?
- What tests do I need?
- What treatments can help?
- What risks does my heart condition create?
- How often will I need follow-up appointments?
- Do I need to restrict my activities?
- Should my children or other first-degree relatives be screened for this condition, and should I meet with a genetic counselor?
- How will other conditions that I have or medicines I take affect my heart condition?
Feel free to ask other questions you have.
What to expect from your doctor
Your healthcare professional is likely to ask you questions such as:
- How severe are your symptoms?
- Have your symptoms changed over time? If so, how?
- Does exercise or physical exertion make your symptoms worse?
- Have you ever fainted?
What you can do in the meantime
Before your appointment, ask your family members if any relatives have been diagnosed with hypertrophic cardiomyopathy or have had unexplained, sudden death.
If exercise makes your symptoms worse, don’t do strenuous exercise until you have seen your healthcare professional. Ask for specific exercise recommendations.


