Pulmonary hypertension
![]() November, 20th, 2024
November, 20th, 2024
Benefit Summary
This lung condition makes the heart work harder and become weak. Changes in genes and some medicines and diseases can cause it. Know if you’re at risk.
Overview
, Overview, ,
Pulmonary hypertension is a type of high blood pressure that affects the arteries in the lungs and the right side of the heart.
In one form of pulmonary hypertension, called pulmonary arterial hypertension (PAH), blood vessels in the lungs are narrowed, blocked or destroyed. The damage slows blood flow through the lungs. Blood pressure in the lung arteries goes up. The heart must work harder to pump blood through the lungs. The extra effort eventually causes the heart muscle to become weak and fail.
In some people, pulmonary hypertension slowly gets worse and can be life-threatening. There’s no cure for pulmonary hypertension. But treatments are available to help you feel better, live longer and improve your quality of life.

When blood vessels in the lungs become thickened, narrowed, blocked or destroyed, it’s harder for blood to flow through the lungs. As a result, blood pressure increases in the lungs. This condition is called pulmonary hypertension.
Pulmonary hypertension Symptoms
The symptoms of pulmonary hypertension develop slowly. You may not notice them for months or even years. Symptoms get worse as the disease progresses.
Pulmonary hypertension symptoms include:
- Shortness of breath, at first while exercising and eventually while at rest.
- Blue or gray skin color due to low oxygen levels. Depending on your skin color, these changes may be harder or easier to see.
- Chest pressure or pain.
- Dizziness or fainting spells.
- Fast pulse or pounding heartbeat.
- Fatigue.
- Swelling in the ankles, legs and belly area.
Shortness of breath is the most common symptom of pulmonary hypertension. But it may be caused by other health conditions such as asthma. See a health care professional for an accurate diagnosis.
Causes
The typical heart has two upper chambers and two lower chambers. Each time blood moves through the heart, the lower right chamber pumps blood to the lungs. The blood passes through a large blood vessel called the pulmonary artery.
Blood usually flows easily through blood vessels in the lungs to the left side of the heart. These blood vessels are the pulmonary arteries, capillaries and veins.
But changes in the cells that line the lung arteries can cause the artery walls to become narrow, stiff, swollen and thick. These changes may slow down or stop blood flow through the lungs, causing pulmonary hypertension.
Pulmonary hypertension is classified into five groups, depending on the cause.
Group 1: Pulmonary arterial hypertension (PAH)
Causes include:
- Unknown cause, called idiopathic pulmonary arterial hypertension.
- Changes in a gene passed down through families, called heritable pulmonary arterial hypertension.
- Use of some medicines or illegal drugs, including methamphetamine.
- Heart problems present at birth, called a congenital heart defect.
- Other health conditions, including scleroderma, lupus and chronic liver disease such as cirrhosis.
Group 2: Pulmonary hypertension caused by left-sided heart disease
This is the most common form of pulmonary hypertension. Causes include:
- Left heart failure.
- Left-sided heart valve disease such as mitral valve or aortic valve disease.
Group 3: Pulmonary hypertension caused by lung disease
Causes include:
- Scarring of the lungs, called pulmonary fibrosis.
- Chronic obstructive pulmonary disease.
- Sleep apnea.
- Long-term exposure to high altitudes in people who may be at higher risk of pulmonary hypertension.
Group 4: Pulmonary hypertension caused by chronic blood clots or blockages in the pulmonary artery
Causes include:
- Chronic blood clots in the lungs, called pulmonary emboli.
- Tumors that block the pulmonary artery.
Group 5: Pulmonary hypertension triggered by other health conditions
Causes include:
- Blood disorders, including polycythemia vera and essential thrombocythemia.
- Inflammatory disorders such as sarcoidosis.
- Metabolic disorders, including glycogen storage disease.
- Kidney disease.
Eisenmenger syndrome and pulmonary hypertension
Eisenmenger syndrome is a type of congenital heart disease that causes pulmonary hypertension. It can occur with unrepaired holes between the heart chambers. An example is a large hole in the heart between the two lower heart chambers called a ventricular septal defect.
The hole in the heart causes blood to flow incorrectly in the heart. Oxygen-rich blood mixes with oxygen-poor blood. The blood then returns to the lungs instead of going to the rest of the body. This increases the blood flow and pressure in the pulmonary arteries, causing pulmonary hypertension.
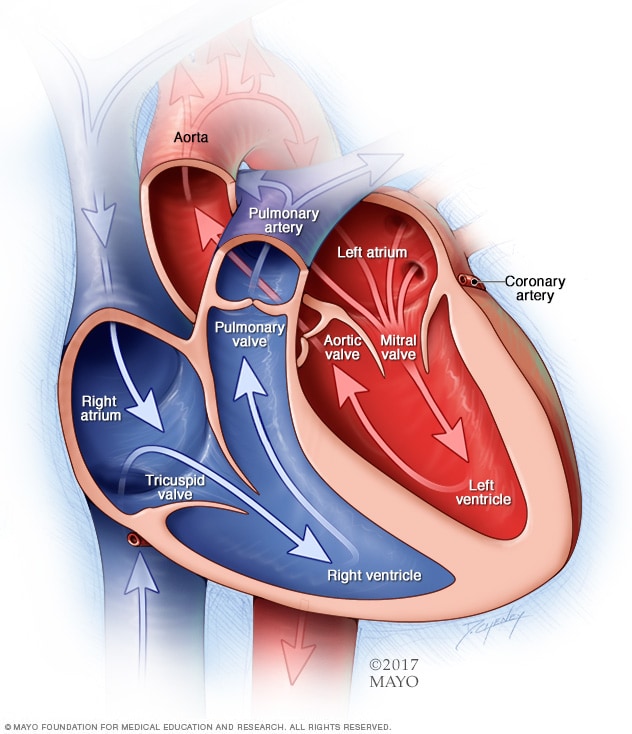
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves are gates at the chamber openings. They keep blood flowing in the right direction.
Chambers and valves of the heart Risk factors
Pulmonary hypertension is usually diagnosed in people ages 30 to 60. Growing older can increase the risk of developing Group 1 pulmonary hypertension, called pulmonary arterial hypertension (PAH). PAH from an unknown cause is more common in younger adults.
Other things that can raise the risk of pulmonary hypertension are:
- A family history of the condition.
- Being overweight.
- Smoking.
- Blood-clotting disorders or a family history of blood clots in the lungs.
- Exposure to asbestos.
- A heart problem that you’re born with, called a congenital heart defect.
- Living at a high altitude.
- Use of certain drugs, including some weight-loss medicines and illegal drugs such as cocaine or methamphetamine.
Complications
Potential complications of pulmonary hypertension include:
-
Right-sided heart enlargement and heart failure. Also called cor pulmonale, this condition causes the heart’s right lower chamber to get larger. The chamber has to pump harder than usual to move blood through narrowed or blocked lung arteries.
As a result, the heart walls thicken. The right lower heart chamber stretches to increase the amount of blood it can hold. These changes create more strain on the heart, and eventually the right lower heart chamber fails.
- Blood clots. Having pulmonary hypertension increases the risk of blood clots in the small arteries in the lungs.
- Irregular heartbeats. Pulmonary hypertension can cause changes in the heartbeat, called arrhythmias, which can be life-threatening.
- Bleeding in the lungs. Pulmonary hypertension can lead to life-threatening bleeding into the lungs and coughing up blood.
- Pregnancy complications. Pulmonary hypertension can be life-threatening for the mother and the developing baby.
Diagnosis
Pulmonary hypertension is hard to diagnose early because it’s not often found during a routine physical exam. Even when pulmonary hypertension is more advanced, its symptoms are similar to those of other heart and lung conditions.
To diagnose pulmonary hypertension, a health care professional examines you and asks about your symptoms. You’ll likely be asked questions about your medical and family history.
Tests
Tests done to help diagnose pulmonary hypertension may include:
- Blood tests. Blood tests can help find the cause of pulmonary hypertension or show signs of complications.
- Chest X-ray. A chest X-ray creates pictures of the heart, lungs and chest. It may be used to check for other lung conditions that can cause pulmonary hypertension.
- Electrocardiogram (ECG or EKG). This simple test records the electrical activity of the heart. It can show changes in the heartbeat.
-
Echocardiogram. Sound waves are used to create moving images of the beating heart. An echocardiogram shows blood flow through the heart. This test may be done to help diagnose pulmonary hypertension or to determine how well treatments are working.
Sometimes, an echocardiogram is done while exercising on a stationary bike or treadmill to learn how activity affects the heart. If you have this test, you may be asked to wear a mask that checks how well the heart and lungs use oxygen and carbon dioxide.
-
Right heart catheterization. If an echocardiogram shows pulmonary hypertension, this test may be done to confirm the diagnosis.
During this procedure, a cardiologist places a thin, flexible tube called a catheter into a blood vessel, usually in the neck. The catheter is gently guided into the lower right heart chamber and the pulmonary artery. A doctor can then measure blood pressure in the main pulmonary arteries and the right ventricle.
Other tests may be done to check the condition of the lungs and pulmonary arteries. The following tests may give more information about the cause of pulmonary hypertension:
- Exercise stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heartbeat is watched. They can show how the heart reacts to exercise.
-
Computerized tomography (CT) scan. This test uses X-rays to create cross-sectional images of specific parts of the body. Dye called contrast may be given into a vein to help the blood vessels show up more clearly on the images.
A heart CT scan, called a cardiac CT scan, can show the size of the heart and any blockages in the pulmonary arteries. It can help diagnose lung diseases that might lead to pulmonary hypertension such as COPD or pulmonary fibrosis.
- Magnetic resonance imaging (MRI). This test uses magnetic fields and radio waves to create detailed images of the heart. It can show blood flow in the pulmonary arteries and determine how well the right lower heart chamber is working.
- Lung function test. For this test, you blow into a special device. The device measures how much air the lungs can hold. It shows how air flows in and out of the lungs.
- Sleep study. A sleep study measures brain activity, heart rate, blood pressure, oxygen levels and other things as you sleep. The test can help diagnose sleep apnea, which can cause pulmonary hypertension.
- Ventilation/perfusion (V/Q) scan. In this test, a radioactive tracer is given through a vein (IV). The tracer shows blood flow. You also may breathe in a tracer that shows airflow to the lungs. A V/Q scan can show whether blood clots are causing symptoms of pulmonary hypertension.
- Lung biopsy. Rarely, a sample of tissue may be taken from the lung to check for a possible cause of pulmonary hypertension.
Genetic testing
Screening for gene changes that cause pulmonary hypertension may be recommended. If you have these gene changes, other family members may need to be screened too.
Pulmonary hypertension functional classification
Once a diagnosis of pulmonary hypertension is confirmed, the condition is classified according to how the symptoms affect you and your ability to do everyday tasks.
Pulmonary hypertension may fall into one of the following groups:
- Class I. Pulmonary hypertension is diagnosed, but there are no symptoms during rest or exercise.
- Class II. There are no symptoms at rest. Everyday chores or activities such as going to work or the grocery store may cause some shortness of breath or mild chest pain. There’s a slight limitation of physical activity.
- Class III. It’s comfortable at rest, but doing simple tasks such as bathing, dressing or preparing meals causes fatigue, shortness of breath and chest pain. The ability to do physical activity becomes very limited.
- Class IV. Symptoms occur at rest and during physical activity. Any type of activity causes increasing discomfort.
Your health care team may use a risk calculator that considers your symptoms and test results to understand what type of treatment is needed. This is called pulmonary hypertension risk stratification.
Treatment
There’s no cure for pulmonary hypertension. But treatment is available to improve symptoms and prolong life, and to keep the disease from getting worse. You also may get treatments for any health problem that might be causing pulmonary hypertension.
It often takes some time to find the most appropriate treatment for pulmonary hypertension. The treatments are often complex. You usually need a lot of health checkups.
Medications
If you have pulmonary hypertension, you may get medicines to treat your symptoms and help you feel better. Medicines also may be used to treat or prevent complications. Treatment may include:
-
Medicines to relax blood vessels. Also called vasodilators, these medicines help open narrowed blood vessels and improve blood flow. The medicine comes in many forms. It may be breathed in, taken by mouth or given by IV. Some types are given continuously through a small pump attached to the body.
Examples of vasodilators to treat pulmonary hypertension include epoprostenol (Flolan, Veletr), treprostinil (Remodulin, Tyvaso, others), Iloprost (Ventavis) and selexipag (Uptravi).
- Soluble guanylate cyclase (sGC) stimulators. This type of medicine relaxes the pulmonary arteries and lowers pressure in the lungs. Examples include riociguat (Adempas). Do not take these medicines if you’re pregnant.
- Medicines to widen blood vessels. Medicines called endothelin receptor antagonists reverse the effect of a substance in the walls of blood vessels that causes them to narrow. Such medicines include bosentan (Tracleer), macitentan (Opsumit) and ambrisentan (Letairis). They may improve energy level and symptoms. Do not take these medicines if you are pregnant.
- Medicines to increase blood flow. Medicines called phosphodiesterase 5 (PDE5) inhibitors may be used to increase blood flow through the lungs. These medicines also are used to treat erectile dysfunction. They include sildenafil (Revatio, Viagra) and tadalafil (Adcirca, Alyq, Cialis).
- High-dose calcium channel blockers. These medicines help relax the muscles in the walls of blood vessels. They include amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and nifedipine (Procardia). Although calcium channel blockers can be effective, only a small number of people with pulmonary hypertension improve while taking them.
- Blood thinners. Also called anticoagulants, these medicines help prevent blood clots. One example is warfarin (Jantoven). Blood-thinning medicines slow the clotting process. The medicines can increase the risk of bleeding. This is especially true if you’re having surgery or a procedure that enters the body or creates an opening in the skin. Talk to your health care team about your risk.
- Digoxin (Lanoxin). This medicine helps the heart beat stronger and pump more blood. It can help control irregular heartbeats.
- Water pills, also called diuretics. These medicines help the kidneys remove excess fluid from the body. This reduces the amount of work the heart has to do. Diuretics also may be used to reduce fluid buildup in the lungs, legs and belly area.
- Oxygen therapy. Breathing pure oxygen is sometimes recommended as a treatment for pulmonary hypertension. This treatment may be suggested if you live at a high altitude or have sleep apnea. Some people with pulmonary hypertension need oxygen therapy all the time.
Surgery or other procedures
If medicines do not help control the symptoms of pulmonary hypertension, surgery may be recommended. Surgeries and procedures to treat pulmonary hypertension may include:
- Atrial septostomy. This treatment may be recommended if medicines don’t control pulmonary hypertension symptoms. In an atrial septostomy, a doctor creates an opening between the upper left and right chambers of the heart. The opening reduces the pressure on the right side of the heart. Potential complications include irregular heartbeats called arrhythmias.
- Lung or heart-lung transplant. Sometimes, a lung or heart-lung transplant may be needed, especially for younger people who have idiopathic pulmonary arterial hypertension. After a transplant, medicine must be taken for life to help reduce the chance of rejection.
Lifestyle and home remedies
Lifestyle changes may help improve pulmonary hypertension symptoms. Try these tips:
- Eat healthy. Eat a healthy diet rich in whole grains, fruits and vegetables, lean meats, and low-fat dairy products. Try to stay away from saturated fat, trans fat and cholesterol. Limit salt.
- Stay as active as possible and manage weight. Even mild forms activity might be too exhausting for some people who have pulmonary hypertension. For others, moderate exercise, such as walking, might be helpful — especially when done during oxygen therapy. Your health care team can help you plan an appropriate exercise program.
- Don’t smoke. If you smoke, the most important thing you can do for your heart and lungs is to stop. If you need support quitting, ask your health care team for treatment that can help. Avoid secondhand smoke too, if possible.
- Get plenty of rest. Resting can reduce tiredness related to pulmonary hypertension.
- Avoid high altitudes. High altitudes can make pulmonary hypertension worse. If you live at an altitude of 8,000 feet (2,438 meters) or higher, you might be told to consider moving to a lower altitude.
- Avoid activities that can excessively lower blood pressure. These include sitting in a hot tub or sauna or taking long hot baths or showers. Such activities lower blood pressure and can cause fainting or even death. Also, do not do activities that cause a lot of straining, such as lifting heavy objects or weights.
- Give your health care team a list of your medicines. Some medicines can make pulmonary hypertension worse or affect its treatment.
- Get regular health checkups. Tell your health care team about any new or worsening symptoms or medicine side effects. If pulmonary hypertension affects your quality of life, ask about options that could help.
- Get recommended vaccines. Respiratory infections can cause serious health concerns for people with pulmonary hypertension. Ask your health care team about recommend vaccines to prevent common viral infections.
- Talk to a health care professional before becoming pregnant. Pulmonary hypertension can cause serious complications to both mother and baby during pregnancy. Birth control pills can increase the risk of blood clots. Talk to your health care team about other birth control options.
Coping and support
Connecting with others who are going through similar situations may help you ease and manage stress. Ask your health care team if there are any pulmonary hypertension support groups in your area.
Preparing for an appointment
If you think that you might have or be at risk of pulmonary hypertension, make an appointment for a health checkup.
There’s often a lot to discuss at your appointment, so it’s a good idea to be prepared. Here’s some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make your appointment, ask if there is anything you need to do before your checkup. For example, you might be told not to eat or drink before some medical tests.
- Write down any symptoms you’re having, including any that might seem unrelated to pulmonary hypertension. Try to remember when they began. Be specific, such as days, weeks and months.
- Make a list of important personal information, including any family history of pulmonary hypertension, lung disease, heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medicines, as well as any vitamins, herbal products or other supplements that you’re taking.
- Take a family member or friend along, if possible. Someone who goes with you can help you remember information you’re given.
- Be prepared to discuss your diet and exercise habits. If you don’t already follow a diet or exercise routine, talk to your health care team about any challenges you might face in getting started.
- Make a list of questions to ask your health care team. List your questions from most important to least important in case time runs out.
For pulmonary hypertension, some basic questions to ask your health care team are:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What kinds of tests do I need?
- What’s the most appropriate treatment?
- Is there a generic alternative to the medicine you’re prescribing?
- What are the options to the primary treatment that you’re suggesting?
- What’s an appropriate level of physical activity?
- How often should I be checked for changes in my condition?
- I have other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a specialist?
- Are there any brochures or other printed material that I can have? What websites do you suggest?
Don’t hesitate to ask other questions.
What to expect from your doctor
Your doctor and other members of your health care team may ask you many questions. Being ready to answer them might give you more time to discuss any concerns. You may be asked:
- When did you first begin having symptoms?
- Do you always have symptoms, or do they come and go?
- How severe are the symptoms?
- What, if anything, seems to improve symptoms?
- What, if anything, seems to make symptoms worse?
What you can do in the meantime
It’s never too late to make healthy lifestyle changes, such as quitting smoking, reducing salt and eating a healthy diet. These changes may help prevent pulmonary hypertension from getting worse.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



