Takayasu's arteritis
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Understand this rare disease that damages the aorta, the large artery that carries blood from your heart to the rest of your body.
Overview
, Overview, ,
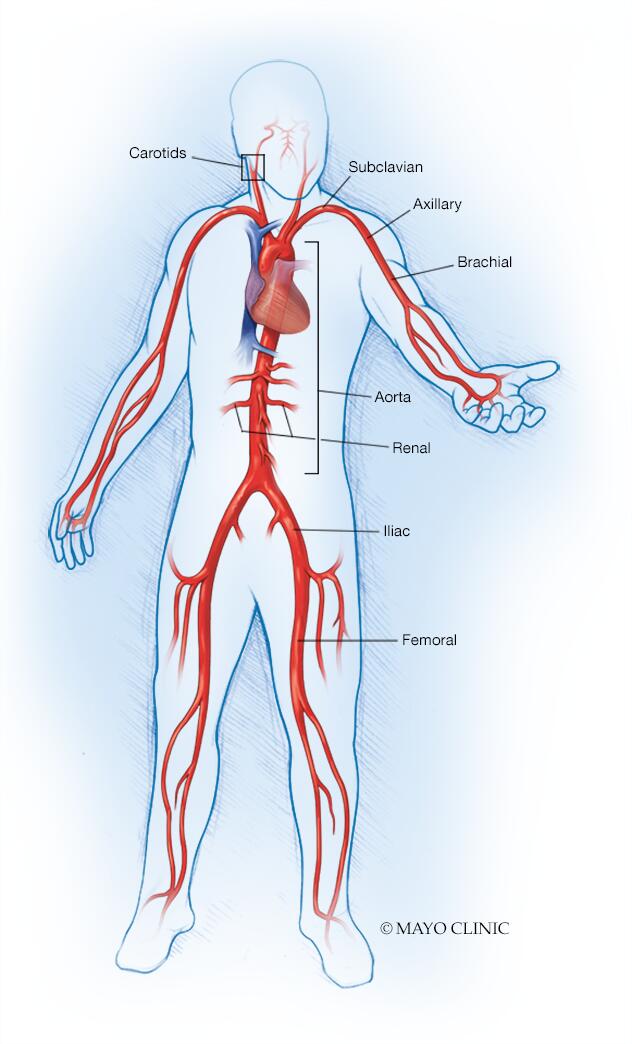
Takayasu’s arteritis (tah-kah-YAH-sooz ahr-tuh-RIE-tis) is a rare type of vasculitis, a group of disorders that causes blood vessel inflammation. In Takayasu’s arteritis, the inflammation damages the large artery that carries blood from your heart to the rest of your body (aorta) and its main branches.
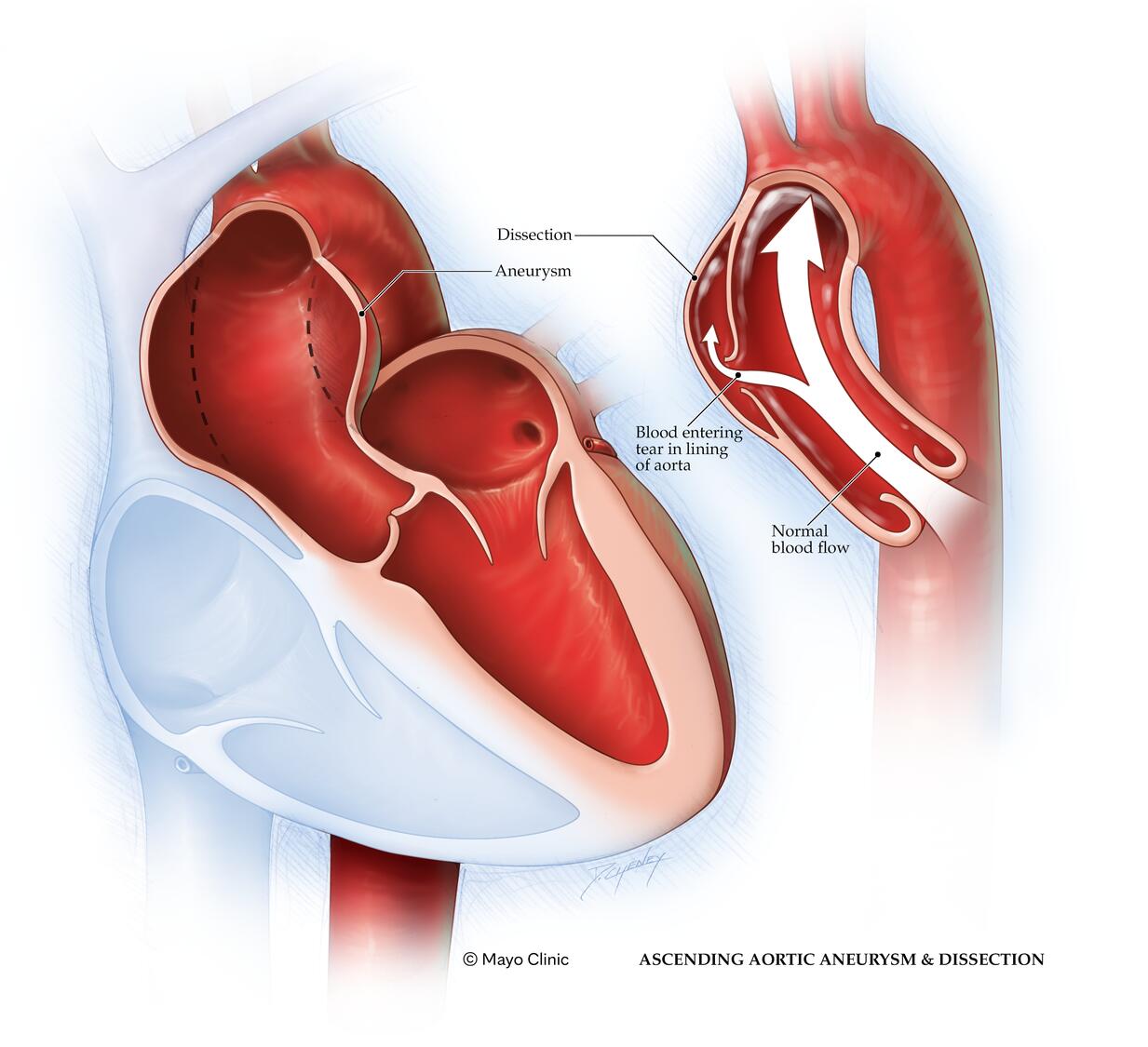
The disease can lead to narrowed or blocked arteries, or to weakened artery walls that may bulge (aneurysm) and tear. It can also lead to arm or chest pain, high blood pressure, and eventually heart failure or stroke.
If you don’t have symptoms, you may not need treatment. But most people with the disease need medications to control inflammation in the arteries and to prevent complications. Even with treatment, relapses are common, and your symptoms may come and go.
The signs and symptoms of Takayasu’s arteritis often occur in two stages.
Stage 1
In the first stage, you’re likely to feel unwell with:
- Fatigue
- Unintended weight loss
- Muscle and joint aches and pains
- Mild fever, sometimes accompanied by night sweats
Not everyone has these early signs and symptoms. It’s possible for inflammation to damage arteries for years before you realize something is wrong.
Stage 2
During the second stage, inflammation causes arteries to narrow so less blood and oxygen and fewer nutrients reach your organs and tissues. Stage 2 signs and symptoms may include:
- Weakness or pain in your limbs with use
- A weak pulse, difficulty getting a blood pressure or a difference in blood pressure between your arms
- Lightheadedness, dizziness or fainting
- Headaches or visual changes
- Memory problems or trouble thinking
- Chest pain or shortness of breath
- High blood pressure
- Diarrhea or blood in your stool
- Too few red blood cells (anemia)
When to see a doctor
Seek immediate medical attention for shortness of breath, chest or arm pain, or signs of a stroke, such as face drooping, arm weakness or having difficulty speaking.
Make an appointment with your doctor if you have other signs or symptoms that worry you. Early detection of Takayasu’s arteritis is key to getting effective treatment.
If you’ve already been diagnosed with Takayasu’s arteritis, keep in mind that your symptoms may come and go even with effective treatment. Pay attention to symptoms similar to those that occurred originally or to any new ones, and be sure to tell your doctor promptly about changes.
Causes
With Takayasu’s arteritis, the aorta and other major arteries, including those leading to your head and kidneys, can become inflamed. Over time the inflammation causes changes in these arteries, including thickening, narrowing and scarring.
No one knows exactly what causes the initial inflammation in Takayasu’s arteritis. The condition is likely an autoimmune disease in which your immune system attacks your own arteries by mistake. The disease may be triggered by a virus or other infection.
Risk factors
Takayasu’s arteritis primarily affects girls and women younger than 40. The disorder occurs worldwide, but it’s most common in Asia. Sometimes the condition runs in families. Researchers have identified certain genes associated with Takayasu’s arteritis.
Complications
With Takayasu’s arteritis, cycles of inflammation and healing in the arteries might lead to one or more of the following complications:
- Hardening and narrowing of blood vessels, which can cause reduced blood flow to organs and tissues.
- High blood pressure, usually as a result of decreased blood flow to your kidneys.
- Inflammation of the heart, which may affect the heart muscle or the heart valves.
- Heart failure due to high blood pressure, inflammation of the heart, an aortic valve that allows blood to leak back into your heart, or a combination of these.
- Stroke, which occurs as a result of reduced or blocked blood flow in arteries leading to your brain.
- Transient ischemic attack (TIA), which is also called a ministroke. serves as a warning sign because it produces symptoms similar to a stroke but doesn’t cause permanent damage.
- Aneurysm in the aorta, which occurs when the walls of the blood vessel weaken and stretch, forming a bulge that has the potential to break.
- Heart attack, which may occur as a result of reduced blood flow to the heart.
Pregnancy
A healthy pregnancy is possible for women with Takayasu’s arteritis. But the disease and drugs used to treat it can affect your fertility and pregnancy. If you have Takayasu’s arteritis and are planning on becoming pregnant, work with your doctor to develop a plan to limit complications of pregnancy before you conceive. See your doctor regularly during your pregnancy for checkups.
Your doctor will ask you about your signs and symptoms, conduct a physical exam, and take your medical history. He or she may also have you undergo some of the following tests and procedures to help rule out other conditions that resemble Takayasu’s arteritis and to confirm the diagnosis. Some of these tests may also be used to check on your progress during treatment.
- Blood tests. These tests can be used to look for signs of inflammation. Your doctor may also check for anemia.
-
X-rays of your blood vessels (angiography). During an angiogram, a long, flexible tube (catheter) is inserted into a large artery or vein. A special contrast dye is then injected into the catheter, and X-rays are taken as the dye fills your arteries or veins.
The resulting images allow your doctor to see if blood is flowing normally or if it’s being slowed or interrupted due to narrowing (stenosis) of a blood vessel. A person with Takayasu’s arteritis generally has several areas of stenosis.
- Magnetic resonance angiography (MRA). This less invasive form of angiography produces detailed images of your blood vessels without the use of catheters or X-rays. MRA works by using radio waves in a strong magnetic field to produce data that a computer turns into detailed images of tissue slices. During this test, a contrast dye is injected into a vein or artery to help your doctor better see and examine the blood vessels.
- Computerized tomography (CT) angiography. This is another noninvasive form of angiography combining computerized analysis of X-ray images with the use of intravenous contrast dye to allow your doctor to check the structure of your aorta and its nearby branches and to monitor blood flow.
- Ultrasonography. Doppler ultrasound, a more sophisticated version of the common ultrasound, has the ability to produce very high-resolution images of the walls of certain arteries, such as those in the neck and shoulder. It may be able to detect subtle changes in these arteries before other imaging techniques can.
- Positron emission tomography (PET). This imaging test is often done in combination with computerized tomography or magnetic resonance imaging. PET can measure the intensity of inflammation in blood vessels. Before the scan, a radioactive drug is injected into a vein or an artery to make it easier for your doctor to see areas of decreased blood flow.
Treatment
Treatment of Takayasu’s arteritis focuses on controlling inflammation with medications and preventing further damage to your blood vessels.
Takayasu’s arteritis can be difficult to treat because the disease may remain active even if your symptoms improve. It’s also possible that irreversible damage has already occurred by the time you’re diagnosed.
On the other hand, if you don’t have signs and symptoms or serious complications, you may not need treatment or you may be able to taper and stop treatment if your doctor recommends it.
Medications
Talk with your doctor about the drug or drug combinations that are options for you and their possible side effects. Your doctor may prescribe:
-
Corticosteroids to control inflammation. The first line of treatment is usually a corticosteroid, such as prednisone (Prednisone Intensol, Rayos). Even if you start feeling better, you may need to continue taking the drug long term. After a few months, your doctor may gradually begin to lower the dose until you reach the lowest dose you need to control inflammation. Eventually your doctor may tell you to stop taking the medication completely.
Possible side effects of corticosteroids include weight gain, increased risk of infection and bone thinning. To help prevent bone loss, your doctor may recommend a calcium supplement and vitamin D.
- Other drugs that suppress the immune system. If your condition doesn’t respond well to corticosteroids or you have trouble as your medication dose is lowered, your doctor may prescribe drugs such as methotrexate (Trexall, Xatmep, others), azathioprine (Azasan, Imuran) and leflunomide (Arava). Some people respond well to medications that were developed for people receiving organ transplants, such as mycophenolate mofetil (CellCept). The most common side effect is an increased risk of infection.
- Medications to regulate the immune system. If you don’t respond to standard treatments, your doctor may suggest drugs that correct abnormalities in the immune system (biologics), although more research is needed. Examples of biologics include etanercept (Enbrel), infliximab (Remicade) and tocilizumab (Actemra). The most common side effect with these drugs is an increased risk of infection.
Surgery
If your arteries become severely narrowed or blocked, you may need surgery to open or bypass these arteries to allow an uninterrupted flow of blood. Often this helps to improve certain symptoms, such as high blood pressure and chest pain. In some cases, though, the narrowing or blockage may happen again, requiring a second procedure.
Also, if you develop large aneurysms, surgery may be needed to prevent them from rupturing.
Surgical options are best performed when inflammation of the arteries has been reduced. They include:
- Bypass surgery. In this procedure, an artery or a vein is removed from a different part of your body and attached to the blocked artery, providing a bypass for blood to flow through. Bypass surgery is usually performed when the narrowing of the arteries is irreversible or when there is significant obstruction to blood flow.
- Blood vessel widening (percutaneous angioplasty). This procedure may be indicated if the arteries are severely blocked. During percutaneous angioplasty, a tiny balloon is threaded through a blood vessel and into the affected artery. Once in place, the balloon is expanded to widen the blocked area, then it’s deflated and removed.
- Aortic valve surgery. Surgical repair or replacement of the aortic valve may be needed if the valve is leaking significantly.
Coping and support
One of the greatest challenges of living with Takayasu’s arteritis may be coping with side effects of your medication. The following suggestions may help:
- Understand your condition. Learn everything you can about Takayasu’s arteritis and its treatment. Know the possible side effects of the drugs you take, and tell your doctor about any changes in your health. Ask your doctor about the benefit of taking low-dose aspirin regularly.
-
Eat a healthy diet. Eating well can help prevent potential problems that can result from your condition and medications, such as high blood pressure, thinning bones and diabetes. Emphasize fresh fruits and vegetables, whole grains, and lean meats and fish, while limiting salt, sugar and alcohol.
If you’re taking a corticosteroid drug, ask your doctor if you need to take a vitamin D or calcium supplement.
- Exercise regularly. Regular aerobic exercise, such as walking, can help prevent bone loss, high blood pressure and diabetes. It also benefits your heart and lungs. In addition, many people find that exercise improves their mood and overall sense of well-being.
- Avoid all tobacco products. It’s important to stop using all forms of tobacco to reduce the risk of injuring your blood vessels and tissues even more.
- Stay up-to-date on vaccines. Your medications may make it harder for your body to fight infection. Talk to your doctor about getting vaccinated against the flu, pneumonia, shingles and other diseases.
Preparing for your appointment
If your primary care doctor suspects that you have Takayasu’s arteritis, he or she may refer you to one or more specialists with experience in helping people with this condition. Takayasu’s arteritis is a rare disorder that can be difficult to diagnose and treat.
You may want to talk with your doctor about a referral to a medical center that specializes in treating vasculitis.
Because appointments can be brief and there’s often a lot of information to discuss, it’s a good idea to be prepared. Here’s some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if you need to do anything in advance, such as restrict your diet.
- List any symptoms you’re experiencing, including any that seem unrelated to the reason for which you scheduled the appointment.
- List key personal information, including major stresses and recent life changes.
- List all medications, vitamins and supplements that you’re taking, including doses.
- Ask a family member or friend to come with you. In addition to offering support, he or she can write down information from your doctor or other clinic staff during the appointment.
- List questions to ask your doctor. Preparing a list of questions can help you make the most of your time together.
For Takayasu’s arteritis, some basic questions to ask include:
- What’s the most likely cause of my symptoms?
- What are other possible causes for my symptoms?
- What tests do I need? Do they require any special preparation?
- Is my condition temporary or long lasting?
- What are my treatment options, and which do you recommend?
- I have another medical condition. How can I best manage these conditions together?
- Do I need to change my diet or restrict my activities in any way?
- Is there a generic alternative to the medicine you’re prescribing?
- What if I can’t or don’t want to take steroids?
- Do you have any brochures or other printed material that I can take with me? What websites do you recommend?
What to expect from your doctor
Your doctor will likely ask you a number of questions, such as:
- When did you first start having symptoms?
- Do you have your symptoms all the time, or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to worsen your symptoms?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



