Esophageal varices
![]() March, 7th, 2025
March, 7th, 2025
Benefit Summary
Learn how to spot and what to do if you experience signs of this serious liver disease complication.
Overview
, Overview, ,
Esophageal varices are enlarged veins in the esophagus, the tube that connects the throat and stomach. Esophageal varices most often happen in people with serious liver diseases.
Esophageal varices form when regular blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren’t designed to carry large volumes of blood. The vessels can leak blood or even burst, causing life-threatening bleeding.
A few medicines and medical procedures are available to help prevent or stop bleeding from esophageal varices.

Esophageal varices are enlarged veins in the esophagus. They’re often due to blocked blood flow through the portal vein. The portal vein carries blood from the intestine, pancreas and spleen to the liver.
Esophageal varices Symptoms
Esophageal varices usually don’t cause symptoms unless they bleed. Symptoms of bleeding esophageal varices include:
- Vomiting large amounts of blood.
- Black, tarry or bloody stools.
- Lightheadedness due to blood loss.
- Loss of consciousness in severe cases.
A healthcare professional might suspect esophageal varices if someone has signs of liver disease or has been diagnosed with liver cirrhosis, including:
- Yellow coloration of your skin and eyes, known as jaundice.
- Easy bleeding or bruising.
- Fluid buildup in your belly, called ascites (uh-SAHY-teez).
When to see a doctor
Make an appointment with a healthcare professional if you have symptoms that worry you. If you’ve been diagnosed with liver disease, ask a care professional about your risk of esophageal varices and what you can do to reduce your risk. Also ask whether you should get a procedure to check for esophageal varices.
If you’ve been diagnosed with esophageal varices, a care professional will likely tell you to watch for signs of bleeding. Bleeding esophageal varices are an emergency. Call 911 or your local emergency services right away if you have black or bloody stools, or bloody vomit.
Causes
Esophageal varices sometimes form when blood flow to the liver is blocked. This is most often caused by scar tissue in the liver due to liver disease, also known as cirrhosis of the liver. The blood flow begins to back up. This increases pressure within the large vein, known as the portal vein, that carries blood to the liver. This is known as portal hypertension.
Portal hypertension forces the blood to seek other pathways through smaller veins, such as those in the lowest part of the esophagus. These thin-walled veins balloon with the added blood. Sometimes they rupture and bleed.
Causes of esophageal varices include:
- Severe liver scarring, called cirrhosis. Several liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cholangitis — can result in cirrhosis.
- A blood clot, also called thrombosis. A blood clot in the portal vein or in a vein that feeds into the portal vein, known as the splenic vein, can cause esophageal varices.
- Parasitic infection. Schistosomiasis is a parasitic infection found in parts of Africa, South America, the Caribbean, the Middle East and East Asia. The parasite can damage the liver, as well as the lungs, intestine, bladder and other organs.
Risk factors
Although many people with advanced liver disease develop esophageal varices, most won’t have bleeding. Esophageal varices are more likely to bleed if you have:
- High portal vein pressure. The risk of bleeding increases as the pressure in the portal vein increases.
- Large varices. The larger the esophageal varices, the more likely they are to bleed.
- Red marks on the varices. Some esophageal varices show long red streaks or red spots. A medical professional can see them through a thin, flexible tube, called an endoscope, passed down the throat. These marks suggest a high risk of bleeding.
- Severe cirrhosis or liver failure. Most often, the more serious the liver disease, the more likely esophageal varices are to bleed.
- Continued alcohol use. The risk of variceal bleeding is far greater for people who continue to drink, especially if the disease is alcohol related.
If someone had bleeding from esophageal varices before, they’re more likely to have varices that bleed again.
Complications
The most serious complication of esophageal varices is bleeding. If a person has a bleeding episode, the risk of another bleeding episode greatly increases. If a person loses enough blood, they can go into shock, which can lead to death.
Prevention
Currently, no treatment can prevent the development of esophageal varices in people with cirrhosis. While beta blocker drugs are effective in preventing bleeding in many people who have esophageal varices, they don’t stop esophageal varices from forming.
If you’ve been diagnosed with liver disease, ask a healthcare professional about strategies to avoid liver disease complications. To keep your liver healthy:
- Don’t drink alcohol. People with liver disease are often advised to stop drinking alcohol, since the liver processes alcohol. Drinking alcohol may stress an already vulnerable liver.
- Eat a healthy diet. Choose a diet that’s full of fruits and vegetables. Select whole grains and lean sources of protein. Reduce the amount of fatty and fried foods you eat.
- Maintain a healthy weight. An excess amount of body fat can damage your liver. Obesity is associated with a greater risk of complications of cirrhosis. Lose weight if you are obese or overweight.
- Use chemicals sparingly and carefully. Follow the directions on household chemicals, such as cleaning supplies and insect sprays. If you work around chemicals, follow all safety precautions. Your liver removes toxins from your body, so give it a break by limiting the amount of toxins it must process.
- Reduce your risk of hepatitis. Sharing needles and having unprotected sex can increase your risk of hepatitis B and C. Protect yourself by abstaining from sex or using a condom if you choose to have sex. Get tested for exposure to hepatitis A, B and C, since infection can make your liver disease worse. Also ask your healthcare professional whether you should be vaccinated for hepatitis A and hepatitis B.
Diagnosis
If someone is diagnosed with cirrhosis, a healthcare professional will then typically screen for esophageal varices. How often screening tests are done depends on someone’s condition. The main tests used to diagnose esophageal varices are:
-
Upper endoscopy. An upper endoscopy uses a tiny camera on the end of a flexible tube to visually examine the upper digestive system. This procedure is the preferred method of screening for esophageal varices. The tiny camera lets a medical professional examine the esophagus, stomach and the beginning of the small intestine, called the duodenum.
The professional doing the endoscopy looks for dilated veins. If found, the enlarged veins are measured and checked for red streaks and red spots, which usually indicate a significant risk of bleeding. Treatment can be performed during the exam.
- Imaging tests. Both abdominal CT scans and Doppler ultrasounds of the splenic and portal veins can suggest the presence of esophageal varices. An ultrasound test called transient elastography may be used to measure scarring in the liver. This can help determine if someone has portal hypertension, which may lead to esophageal varices.
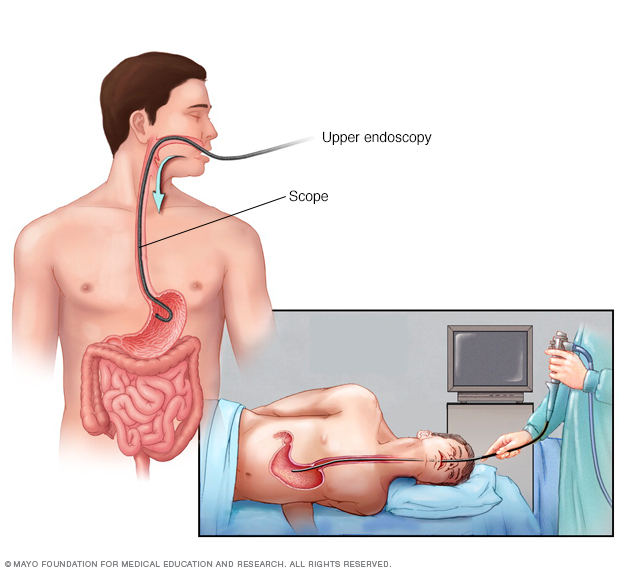
An upper gastrointestinal endoscopy involves inserting a flexible, lighted tube called an endoscope down your throat and into your esophagus. A tiny camera on the end of the endoscope lets your doctor examine your esophagus, stomach and the beginning of your small intestine, called the duodenum.
Endoscopy Treatment
The primary aim in treating esophageal varices is to prevent bleeding. Bleeding esophageal varices are life-threatening. If bleeding happens, treatments are available to try to stop the bleeding.
Treatment to prevent bleeding
Treatments to lower blood pressure in the portal vein may reduce the risk of bleeding esophageal varices. Treatments may include:
- Medicines to reduce pressure in the portal vein. A type of blood pressure drug called a beta blocker may help reduce blood pressure in the portal vein. This can decrease the likelihood of bleeding. Beta blocker medicines include propranolol (Inderal, Innopran XL) and nadolol.
-
Using elastic bands to tie off bleeding veins. If the esophageal varices appear to have a high risk of bleeding, or if the varices have bled before, a healthcare professional might recommend a procedure called endoscopic band ligation.
Using an endoscope, the care professional uses suction to pull the varices into a chamber at the end of the scope and wraps them with an elastic band. This essentially “strangles” the veins so they can’t bleed. Endoscopic band ligation carries a small risk of complications, such as bleeding and scarring of the esophagus.
Treatment if you’re bleeding
Bleeding esophageal varices are life-threatening, and immediate treatment is essential. Treatments used to stop bleeding and reverse the effects of blood loss include:
- Using elastic bands to tie off bleeding veins. A healthcare professional may wrap elastic bands around the esophageal varices during an endoscopy.
- Medicines to slow blood flow into the portal vein. Medicines such as octreotide (Sandostatin) and vasopressin (Vasostrict) slow the flow of blood to the portal vein. Medicine is usually continued for up to five days after a bleeding episode.
-
Diverting blood flow away from the portal vein. If medicine and endoscopy treatments don’t stop the bleeding, a care professional might recommend a procedure called transjugular intrahepatic portosystemic shunt (TIPS).
The shunt is an opening that is created between the portal vein and the hepatic vein, which carries blood from the liver to the heart. The shunt reduces pressure in the portal vein and often stops bleeding from esophageal varices.
But TIPS can cause serious complications, including liver failure and mental confusion. These symptoms can develop when toxins that the liver typically would filter are passed through the shunt directly into the bloodstream.
TIPS is mainly used when all other treatments have failed or as a temporary measure in people awaiting a liver transplant.
-
Placing pressure on varices to stop bleeding. If medicine and endoscopy treatments don’t work, a care professional may try to stop bleeding by applying pressure to the esophageal varices. One way to temporarily stop bleeding is by inflating a balloon to put pressure on the varices for up to 24 hours, a procedure called balloon tamponade. Balloon tamponade is a temporary measure before other treatments can be performed, such as TIPS.
This procedure carries a high risk of bleeding recurrence after the balloon is deflated. Balloon tamponade also may cause serious complications, including a rupture in the esophagus, which can lead to death.
- Restoring blood volume. A transfusion may be needed to replace lost blood, and a clotting factor may be given to stop bleeding.
- Preventing infection. There is an increased risk of infection with bleeding, so an antibiotic may be prescribed to prevent infection.
- Replacing the diseased liver with a healthy one. Liver transplant is an option for people with severe liver disease or those who experience recurrent bleeding of esophageal varices. Although liver transplantation is often successful, the number of people awaiting transplants far outnumbers the available organs.
Rebleeding
There is a high risk that bleeding will recur in people who’ve had bleeding from esophageal varices. Beta blockers and endoscopic band ligation are the recommended treatments to help prevent rebleeding.
After initial banding treatment, a healthcare professional will repeat an upper endoscopy at regular intervals. If necessary, more banding may be done until the esophageal varices are gone or are small enough to reduce the risk of further bleeding.
Potential future treatment
Researchers are exploring an experimental emergency therapy to stop bleeding from esophageal varices that involves spraying an adhesive powder. The hemostatic powder is given through a catheter during an endoscopy. When sprayed on the esophagus, hemostatic powder sticks to the varices and may stop bleeding.
Another possible way to stop bleeding when all other measures fail is to use self-expanding metal stents (SEMS). SEMS can be placed during an endoscopy and stop bleeding by placing pressure on the bleeding esophageal varices.
However, SEMS could damage tissue and can migrate after being placed. The stent should be removed within seven days and bleeding could recur. This option is experimental and isn’t yet widely available.
Preparing for an appointment
You might start by seeing someone on your primary healthcare team. Or you may be referred immediately to a healthcare professional who specializes in digestive disorders, called a gastroenterologist. If you’re having symptoms of internal bleeding, call 911 or your local emergency number to be taken to the hospital for urgent care.
Here’s some information to help you get ready for an appointment.
What you can do
When you make the appointment, ask if there’s anything you need to do in advance, such as fasting before a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes or recent travels, family and personal medical history, and your alcohol use.
- All medicines, vitamins or other supplements you take, including doses.
- Questions to ask during your appointment.
Take a family member or friend along, if possible, to help you remember information you’re given.
For esophageal varices, questions to ask include:
- What’s likely causing my symptoms?
- What other possible causes are there?
- What tests do I need?
- What’s the best course of action?
- What are the side effects of the treatments?
- Are my symptoms likely to recur, and what can I do to prevent that?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Are there brochures or other printed materials I can have? What websites do you recommend?
Don’t hesitate to ask other questions.
What to expect from your doctor
You’ll likely be asked a few questions, such as:
- When did your symptoms begin?
- Have your symptoms stayed the same or gotten worse?
- How severe are your symptoms?
- Have you had signs of bleeding, such as blood in your stools or vomit?
- Have you had hepatitis or yellowing of your eyes or skin (jaundice)?
- Have you traveled recently? Where?
- If you drink alcohol, when did you start and how much do you drink?
What you can do in the meantime
If you develop bloody vomit or stools while you’re waiting for your appointment, call 911 or your local emergency number or go to an emergency room immediately.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



