Ear infection (middle ear)
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
These usually get better on their own, but sometimes medicine is needed. Find out more about how doctors diagnose and treat this common ear condition.
Overview
, Overview, ,
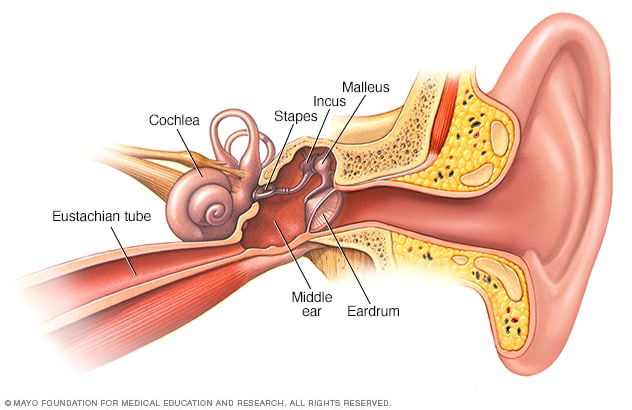
An ear infection (sometimes called acute otitis media) is an infection of the middle ear, the air-filled space behind the eardrum that contains the tiny vibrating bones of the ear. Children are more likely than adults to get ear infections.
Because ear infections often clear up on their own, treatment may begin with managing pain and monitoring the problem. Sometimes, antibiotics are used to clear the infection. Some people are prone to having multiple ear infections. This can cause hearing problems and other serious complications.
The onset of signs and symptoms of ear infection is usually rapid.
Children
Signs and symptoms common in children include:
- Ear pain, especially when lying down
- Tugging or pulling at an ear
- Trouble sleeping
- Crying more than usual
- Fussiness
- Trouble hearing or responding to sounds
- Loss of balance
- Fever of 100 F (38 C) or higher
- Drainage of fluid from the ear
- Headache
- Loss of appetite
Adults
Common signs and symptoms in adults include:
- Ear pain
- Drainage of fluid from the ear
- Trouble hearing
When to see a doctor
Signs and symptoms of an ear infection can indicate several conditions. It’s important to get an accurate diagnosis and prompt treatment. Call your child’s doctor if:
- Symptoms last for more than a day
- Symptoms are present in a child less than 6 months of age
- Ear pain is severe
- Your infant or toddler is sleepless or irritable after a cold or other upper respiratory infection
- You observe a discharge of fluid, pus or bloody fluid from the ear
Causes
An ear infection is caused by a bacterium or virus in the middle ear. This infection often results from another illness — cold, flu or allergy — that causes congestion and swelling of the nasal passages, throat and eustachian tubes.
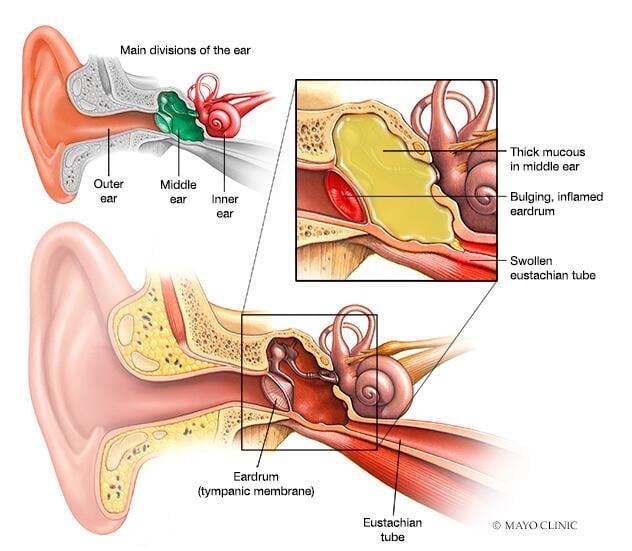
Role of eustachian tubes
The eustachian tubes are a pair of narrow tubes that run from each middle ear to high in the back of the throat, behind the nasal passages. The throat end of the tubes open and close to:
- Regulate air pressure in the middle ear
- Refresh air in the ear
- Drain normal secretions from the middle ear
Swollen eustachian tubes can become blocked, causing fluids to build up in the middle ear. This fluid can become infected and cause the symptoms of an ear infection.
In children, the eustachian tubes are narrower and more horizontal, which makes them more difficult to drain and more likely to get clogged.
Role of adenoids
Adenoids are two small pads of tissues high in the back of the nose believed to play a role in immune system activity.
Because adenoids are near the opening of the eustachian tubes, swelling of the adenoids may block the tubes. This can lead to middle ear infection. Swelling and irritation of adenoids is more likely to play a role in ear infections in children because children have relatively larger adenoids compared to adults.
Related conditions
Conditions of the middle ear that may be related to an ear infection or result in similar middle ear problems include:
- Otitis media with effusion, or swelling and fluid buildup (effusion) in the middle ear without bacterial or viral infection. This may occur because the fluid buildup persists after an ear infection has gotten better. It may also occur because of some dysfunction or noninfectious blockage of the eustachian tubes.
- Chronic otitis media with effusion, occurs when fluid remains in the middle ear and continues to return without bacterial or viral infection. This makes children susceptible to new ear infections and may affect hearing.
- Chronic suppurative otitis media, an ear infection that doesn’t go away with the usual treatments. This can lead to a hole in the eardrum.
Risk factors for ear infections include:
- Age. Children between the ages of 6 months and 2 years are more susceptible to ear infections because of the size and shape of their eustachian tubes and because their immune systems are still developing.
- Group child care. Children cared for in group settings are more likely to get colds and ear infections than are children who stay home. The children in group settings are exposed to more infections, such as the common cold.
- Infant feeding. Babies who drink from a bottle, especially while lying down, tend to have more ear infections than do babies who are breast-fed.
- Seasonal factors. Ear infections are most common during the fall and winter. People with seasonal allergies may have a greater risk of ear infections when pollen counts are high.
- Poor air quality. Exposure to tobacco smoke or high levels of air pollution can increase the risk of ear infections.
- Alaska Native heritage. Ear infections are more common among Alaska Natives.
- Cleft palate. Differences in the bone structure and muscles in children who have cleft palates may make it more difficult for the eustachian tube to drain.
Complications
Most ear infections don’t cause long-term complications. Ear infections that happen again and again can lead to serious complications:
- Impaired hearing. Mild hearing loss that comes and goes is fairly common with an ear infection, but it usually gets better after the infection clears. Ear infections that happen again and again, or fluid in the middle ear, may lead to more-significant hearing loss. If there is some permanent damage to the eardrum or other middle ear structures, permanent hearing loss may occur.
- Speech or developmental delays. If hearing is temporarily or permanently impaired in infants and toddlers, they may experience delays in speech, social and developmental skills.
- Spread of infection. Untreated infections or infections that don’t respond well to treatment can spread to nearby tissues. Infection of the mastoid, the bony protrusion behind the ear, is called mastoiditis. This infection can result in damage to the bone and the formation of pus-filled cysts. Rarely, serious middle ear infections spread to other tissues in the skull, including the brain or the membranes surrounding the brain (meningitis).
- Tearing of the eardrum. Most eardrum tears heal within 72 hours. In some cases, surgical repair is needed.
Prevention
The following tips may reduce the risk of developing ear infections:
- Prevent common colds and other illnesses. Teach your children to wash their hands frequently and thoroughly and to not share eating and drinking utensils. Teach your children to cough or sneeze into their elbow. If possible, limit the time your child spends in group child care. A child care setting with fewer children may help. Try to keep your child home from child care or school when ill.
- Avoid secondhand smoke. Make sure that no one smokes in your home. Away from home, stay in smoke-free environments.
- Breast-feed your baby. If possible, breast-feed your baby for at least six months. Breast milk contains antibodies that may offer protection from ear infections.
- If you bottle-feed, hold your baby in an upright position. Avoid propping a bottle in your baby’s mouth while he or she is lying down. Don’t put bottles in the crib with your baby.
- Talk to your doctor about vaccinations. Ask your doctor about what vaccinations are appropriate for your child. Seasonal flu shots, pneumococcal and other bacterial vaccines may help prevent ear infections.
Diagnosis
Your doctor can usually diagnose an ear infection or another condition based on the symptoms you describe and an exam. The doctor will likely use a lighted instrument (an otoscope) to look at the ears, throat and nasal passage. He or she will also likely listen to your child breathe with a stethoscope.
Pneumatic otoscope
An instrument called a pneumatic otoscope is often the only specialized tool a doctor needs to diagnose an ear infection. This instrument enables the doctor to look in the ear and judge whether there is fluid behind the eardrum. With the pneumatic otoscope, the doctor gently puffs air against the eardrum. Normally, this puff of air would cause the eardrum to move. If the middle ear is filled with fluid, your doctor will observe little to no movement of the eardrum.
Additional tests
Your doctor may perform other tests if there is any doubt about a diagnosis, if the condition hasn’t responded to previous treatments, or if there are other long-term or serious problems.
- Tympanometry. This test measures the movement of the eardrum. The device, which seals off the ear canal, adjusts air pressure in the canal, which causes the eardrum to move. The device measures how well the eardrum moves and provides an indirect measure of pressure within the middle ear.
- Acoustic reflectometry. This test measures how much sound is reflected back from the eardrum — an indirect measure of fluids in the middle ear. Normally, the eardrum absorbs most of the sound. However, the more pressure there is from fluid in the middle ear, the more sound the eardrum will reflect.
- Tympanocentesis. Rarely, a doctor may use a tiny tube that pierces the eardrum to drain fluid from the middle ear — a procedure called tympanocentesis. The fluid is tested for viruses and bacteria. This can be helpful if an infection hasn’t responded well to previous treatments.
- Other tests. If your child has had multiple ear infections or fluid buildup in the middle ear, your doctor may refer you to a hearing specialist (audiologist), speech therapist or developmental therapist for tests of hearing, speech skills, language comprehension or developmental abilities.
What a diagnosis means
- Acute otitis media. The diagnosis of “ear infection” is generally shorthand for acute otitis media. Your doctor likely makes this diagnosis if he or she sees signs of fluid in the middle ear, if there are signs or symptoms of an infection, and if symptoms started relatively suddenly.
- Otitis media with effusion. If the diagnosis is otitis media with effusion, the doctor has found evidence of fluid in the middle ear, but there are presently no signs or symptoms of infection.
- Chronic suppurative otitis media. If the doctor makes a diagnosis of chronic suppurative otitis media, he or she has found that a long-term ear infection resulted in tearing of the eardrum. This is usually associated with pus draining from the ear.
Treatment
Some ear infections resolve without antibiotic treatment. What’s best for your child depends on many factors, including your child’s age and the severity of symptoms.
A wait-and-see approach
Symptoms of ear infections usually improve within the first couple of days, and most infections clear up on their own within one to two weeks without any treatment. The American Academy of Pediatrics and the American Academy of Family Physicians recommend a wait-and-see approach as one option for:
- Children 6 to 23 months with mild middle ear pain in one ear for less than 48 hours and a temperature less than 102.2 F (39 C)
- Children 24 months and older with mild middle ear pain in one or both ears for less than 48 hours and a temperature less than 102.2 F (39 C)
Some evidence suggests that treatment with antibiotics might be helpful for certain children with ear infections. On the other hand, using antibiotics too often can cause bacteria to become resistant to the medicine. Talk with your doctor about the potential benefits and risks of using antibiotics.
Managing pain
Your doctor will advise you on treatments to lessen pain from an ear infection. These may include the following:
- Pain medication. Your doctor may advise the use of over-the-counter acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others) to relieve pain. Use the drugs as directed on the label. Use caution when giving aspirin to children or teenagers. Children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin because aspirin has been linked with Reye’s syndrome. Talk to your doctor if you have concerns.
- Anesthetic drops. These may be used to relieve pain if the eardrum doesn’t have a hole or tear in it.
Antibiotic therapy
After an initial observation period, your doctor may recommend antibiotic treatment for an ear infection in the following situations:
- Children 6 months and older with moderate to severe ear pain in one or both ears for at least 48 hours or a temperature of 102.2 F (39 C) or higher
- Children 6 to 23 months with mild middle ear pain in one or both ears for less than 48 hours and a temperature less than 102.2 F (39 C)
- Children 24 months and older with mild middle ear pain in one or both ears for less than 48 hours and a temperature less than 102.2 F (39 C)
Children younger than 6 months of age with confirmed acute otitis media are more likely to be treated with antibiotics without the initial observational waiting time.
Even after symptoms have improved, be sure to use the antibiotic as directed. Failing to take all the medicine can lead to recurring infection and resistance of bacteria to antibiotic medications. Talk with your doctor or pharmacist about what to do if you accidentally miss a dose.
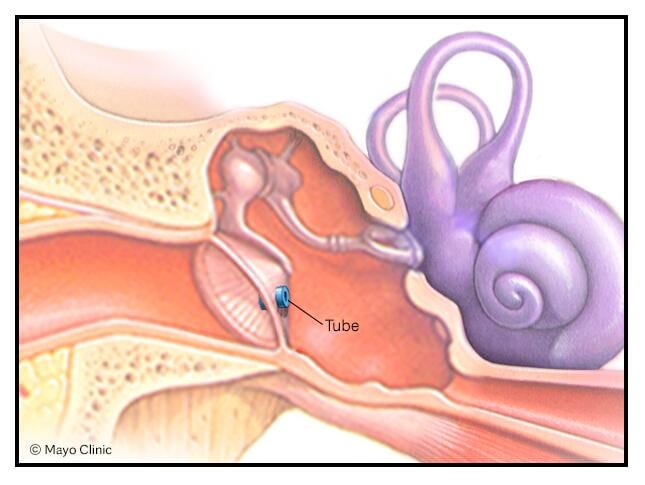
Ear tubes
If your child has certain conditions, your child’s doctor may recommend a procedure to drain fluid from the middle ear. If your child has repeated, long-term ear infections (chronic otitis media) or continuous fluid buildup in the ear after an infection cleared up (otitis media with effusion), your child’s doctor may suggest this procedure.
During an outpatient surgical procedure called a myringotomy, a surgeon creates a tiny hole in the eardrum that enables him or her to suction fluids out of the middle ear. A tiny tube (tympanostomy tube) is placed in the opening to help ventilate the middle ear and prevent the buildup of more fluids. Some tubes are intended to stay in place for four to 18 months and then fall out on their own. Other tubes are designed to stay in longer and may need to be surgically removed.
The eardrum usually closes up again after the tube falls out or is removed.
Treatment for chronic suppurative otitis media
Chronic infection that results in a hole or tear in the eardrum — called chronic suppurative otitis media — is difficult to treat. It’s often treated with antibiotics administered as drops. You may receive instructions on how to suction fluids out through the ear canal before administering drops.
Monitoring
Children who have frequent infections or who have persistent fluid in the middle ear will need to be monitored closely. Talk to your doctor about how often you should schedule follow-up appointments. Your doctor may recommend regular hearing and language tests.
You’ll likely begin by seeing your family doctor or your child’s pediatrician. You may be referred to a specialist in ear, nose and throat (ENT) disorders if the problem has persisted for some time, is not responding to treatment or has occurred frequently.
If your child is old enough to respond, before your appointment talk to the child about questions the doctor may ask and be prepared to answer questions on behalf of your child. Questions for adults will address most of the same issues.
- What signs or symptoms have you noticed?
- When did the symptoms begin?
- Is there ear pain? How would you describe the pain — mild, moderate or severe?
- Have you observed possible signs of pain in your infant or toddler, such as ear pulling, difficulty sleeping or unusual irritability?
- Has your child had a fever?
- Has there been any discharge from the ear? Is the discharge clear, cloudy or bloody?
- Have you observed any hearing impairment? Does your child respond to quiet sounds? Does your older child ask “What?” frequently?
- Has your child recently had a cold, flu or other respiratory symptoms?
- Does your child have seasonal allergies?
- Has your child had an ear infection in the past? When?
- Is your child allergic to any medication, such as amoxicillin?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



