Sore throat
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Find out what causes this common affliction, when to see a doctor and what you can do to get relief from a sore throat.
Overview
, Overview, ,
A sore throat is pain, scratchiness or irritation of the throat that often worsens when you swallow. The most common cause of a sore throat (pharyngitis) is a viral infection, such as a cold or the flu. A sore throat caused by a virus resolves on its own.
Strep throat (streptococcal infection), a less common type of sore throat caused by bacteria, requires treatment with antibiotics to prevent complications. Other less common causes of sore throat might require more complex treatment.
Symptoms
Symptoms of a sore throat can vary depending on the cause. Signs and symptoms might include:
- Pain or a scratchy sensation in the throat
- Pain that worsens with swallowing or talking
- Difficulty swallowing
- Sore, swollen glands in your neck or jaw
- Swollen, red tonsils
- White patches or pus on your tonsils
- A hoarse or muffled voice
Infections causing a sore throat might result in other signs and symptoms, including:
- Fever
- Cough
- Runny nose
- Sneezing
- Body aches
- Headache
- Nausea or vomiting
Take your child to a doctor if your child’s sore throat doesn’t go away with the first drink in the morning, recommends the American Academy of Pediatrics.
Get immediate care if your child has severe signs and symptoms such as:
- Difficulty breathing
- Difficulty swallowing
- Unusual drooling, which might indicate an inability to swallow
If you’re an adult, see your doctor if you have a sore throat and any of the following associated problems, according to the American Academy of Otolaryngology — Head and Neck Surgery:
- A sore throat that is severe or lasts longer than a week
- Difficulty swallowing
- Difficulty breathing
- Difficulty opening your mouth
- Joint pain
- Earache
- Rash
- Fever higher than 101 F (38.3 C)
- Blood in your saliva or phlegm
- Frequently recurring sore throats
- A lump in your neck
- Hoarseness lasting more than two weeks
- Swelling in your neck or face
Causes
Viruses that cause the common cold and the flu also cause most sore throats. Less often, bacterial infections cause sore throats.
Viral infections
Viral illnesses that cause a sore throat include:
- Common cold
- Flu (influenza)
- Mono (mononucleosis)
- Measles
- Chickenpox
- Coronavirus disease 2019 (COVID-19)
- Croup — a common childhood illness characterized by a harsh, barking cough
Bacterial infections
Many bacterial infections can cause a sore throat. The most common is Streptococcus pyogenes (group A streptococcus) which causes strep throat.
Other causes
Other causes of a sore throat include:
- Allergies. Allergies to pet dander, molds, dust and pollen can cause a sore throat. The problem may be complicated by postnasal drip, which can irritate and inflame the throat.
- Dryness. Dry indoor air can make your throat feel rough and scratchy. Breathing through your mouth — often because of chronic nasal congestion — also can cause a dry, sore throat.
- Irritants. Outdoor air pollution and indoor pollution such as tobacco smoke or chemicals can cause a chronic sore throat. Chewing tobacco, drinking alcohol and eating spicy foods also can irritate your throat.
- Muscle strain. You can strain muscles in your throat by yelling, talking loudly or talking for long periods without rest.
-
Gastroesophageal reflux disease (GERD). GERD is a digestive system disorder in which stomach acids back up in the food pipe (esophagus).
Other signs or symptoms may include heartburn, hoarseness, regurgitation of stomach contents and the sensation of a lump in your throat.
-
HIV infection. A sore throat and other flu-like symptoms sometimes appear early after someone is infected with HIV.
Also, someone who is HIV-positive might have a chronic or recurring sore throat due to a fungal infection called oral thrush or due to a viral infection called cytomegalovirus (CMV), which can be serious in people with compromised immune systems.
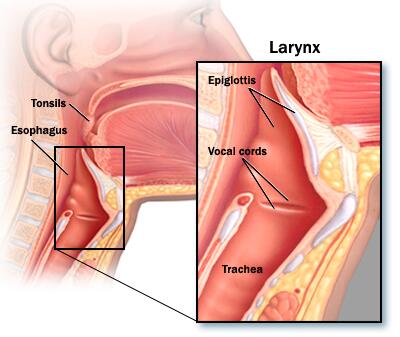
- Tumors. Cancerous tumors of the throat, tongue or voice box (larynx) can cause a sore throat. Other signs or symptoms may include hoarseness, difficulty swallowing, noisy breathing, a lump in the neck, and blood in saliva or phlegm.
Rarely, an infected area of tissue (abscess) in the throat or swelling of the small cartilage “lid” that covers the windpipe (epiglottitis) can cause a sore throat. Both can block the airway, creating a medical emergency.
Risk factors
Although anyone can get a sore throat, some factors make you more susceptible, including:
- Age. Children and teens are most likely to develop sore throats. Children ages 3 to 15 are also more likely to have strep throat, the most common bacterial infection associated with a sore throat.
- Exposure to tobacco smoke. Smoking and secondhand smoke can irritate the throat. The use of tobacco products also increases the risk of cancers of the mouth, throat and voice box.
- Allergies. Seasonal allergies or ongoing allergic reactions to dust, molds or pet dander make developing a sore throat more likely.
- Exposure to chemical irritants. Particles in the air from burning fossil fuels and common household chemicals can cause throat irritation.
- Chronic or frequent sinus infections. Drainage from your nose can irritate your throat or spread infection.
- Close quarters. Viral and bacterial infections spread easily anywhere people gather, whether in child care centers, classrooms, offices or airplanes.
- Weakened immunity. You’re more susceptible to infections in general if your resistance is low. Common causes of lowered immunity include HIV, diabetes, treatment with steroids or chemotherapy drugs, stress, fatigue, and poor diet.
Prevention
The best way to prevent sore throats is to avoid the germs that cause them and practice good hygiene. Follow these tips and teach your child to do the same:
- Wash your hands thoroughly and frequently for at least 20 seconds, especially after using the toilet, before and after eating, and after sneezing or coughing.
- Avoid touching your face. Avoid touching your eyes, nose or mouth.
- Avoid sharing food, drinking glasses or utensils.
- Cough or sneeze into a tissue and throw it away, and then wash your hands. When necessary, sneeze into your elbow.
- Use alcohol-based hand sanitizers as an alternative to washing hands when soap and water aren’t available.
- Avoid touching public phones or drinking fountains with your mouth.
- Regularly clean and disinfect phones, doorknobs, light switches, remotes and computer keyboards. When you travel, clean phones, light switches and remotes in your hotel room.
- Avoid close contact with people who are sick or have symptoms.
Diagnosis
Your or your child’s doctor may review the symptoms and medical history. He or she may conduct a physical exam that includes:
- Using a lighted instrument to look at the throat, and likely the ears and nasal passages
- Gently feeling the neck to check for swollen glands (lymph nodes)
- Listening to your or your child’s breathing with a stethoscope
Throat swab
In many cases, doctors use a simple test to detect streptococcal bacteria, the cause of strep throat. The doctor rubs a sterile swab over the back of the throat to get a sample of secretions and sends the sample to a lab for testing. Many clinics are equipped with a lab that can get a test result for a rapid antigen test within a few minutes. However, a second, often more reliable test, called a throat culture, is sometimes sent to a lab that returns results within 24 to 48 hours.
Rapid antigen tests aren’t as sensitive, although they can detect strep bacteria quickly. Because of this, the doctor may send a throat culture to a lab to test for strep throat if the antigen test comes back negative.
In some cases, doctors may use a molecular test to detect streptococcal bacteria. In this test, a doctor swipes a sterile swab over the back of the throat to get a sample of secretions. The sample is tested in a lab. Your or your child’s doctor may have accurate results within a few minutes.
Treatment
A sore throat caused by a viral infection usually lasts five to seven days and doesn’t usually require medical treatment. Antibiotics don’t help treat a viral infection.
To ease pain and fever, many people turn to acetaminophen (Tylenol, others) or other mild pain relievers.
Consider giving your child over-the-counter pain medications designed for infants or children, such as acetaminophen (Children’s Tylenol, FeverAll, others) or ibuprofen (Children’s Advil, Children’s Motrin, others), to ease symptoms.
Never give aspirin to children or teenagers because it has been linked to Reye’s syndrome, a rare but potentially life-threatening condition that causes swelling in the liver and brain.
Treating bacterial infections
If your or your child’s sore throat is caused by a bacterial infection, your doctor or pediatrician will prescribe antibiotics.
You or your child must take the full course of antibiotics as prescribed even if the symptoms are gone. Failure to take all of the medication as directed can result in the infection worsening or spreading to other parts of the body.
Not completing the full course of antibiotics to treat strep throat can increase a child’s risk of rheumatic fever or serious kidney inflammation.
Talk to your doctor or pharmacist about what to do if you forget a dose.
Other treatments
If a sore throat is a symptom of a condition other than a viral or bacterial infection, other treatments will likely be considered depending on the diagnosis.
Self care
Regardless of the cause of your sore throat, these at-home care strategies can help you ease your or your child’s symptoms:
- Rest. Get plenty of sleep. Rest your voice, too.
- Drink fluids. Fluids keep the throat moist and prevent dehydration. Avoid caffeine and alcohol, which can dehydrate you.
- Try comforting foods and beverage. Warm liquids — broth, caffeine-free tea or warm water with honey — and cold treats such as ice pops can soothe a sore throat. Don’t give honey to children younger than age 1.
- Gargle with saltwater. A saltwater gargle of 1/4 to 1/2 teaspoon (1250 to 2500 milligrams) of table salt to 4 to 8 ounces (120 to 240 milliliters) of warm water can help soothe a sore throat. Children older than 6 and adults can gargle the solution and then spit it out.
- Humidify the air. Use a cool-air humidifier to eliminate dry air that may further irritate a sore throat, being sure to clean the humidifier regularly so it doesn’t grow mold or bacteria. Or sit for several minutes in a steamy bathroom.
- Consider lozenges or hard candy. Either can soothe a sore throat, but don’t give them to children age 4 and younger because of choking risk.
- Avoid irritants. Keep your home free from cigarette smoke and cleaning products that can irritate the throat.
- Stay at home until you’re no longer sick. This can help protect others from catching a cold or other virus.
Alternative medicine
Although several alternative treatments are commonly used to soothe a sore throat, evidence is limited about what works. If you or your child needs an antibiotic for a bacterial infection, don’t rely on alternative treatments alone.
Check with your doctor before using any herbal remedies, as they can interact with prescription medications and may not be safe for children, pregnant and breastfeeding women, and people with certain health conditions.
Herbal or alternative products for a sore throat are often packaged as teas, sprays or lozenges. Common alternative remedies include:
- Slippery elm
- Licorice root
- Marshmallow root
Preparing for your appointment
If you or your child has a sore throat, make an appointment with your family doctor or your child’s pediatrician. In some cases, you may be referred to a specialist in ear, nose and throat (ENT) disorders or an allergy specialist (allergist).
Here’s some information to help you get ready for your appointment.
What you can do
Make a list of:
- Symptoms you or your child has, and for how long
- Key personal information, such as recent contact with someone who was ill
- All medications, vitamins or other supplements you or your child takes, including doses
- Questions to ask the doctor
For a sore throat, some basic questions to ask your doctor include:
- What’s likely causing these symptoms?
- Are there other possible causes?
- What tests are needed?
- What treatment do you recommend?
- How soon do you expect symptoms to improve with treatment?
- How long will this be contagious? When is it safe to return to school or work?
- What self-care steps might help?
Don’t hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask questions about you or your child. Your doctor might ask:
- Are there symptoms other than a sore throat?
- Have these symptoms included a fever? How high?
- Has there been difficulty breathing?
- Does anything worsen the sore throat, such as swallowing?
- Does anything seem to make the symptoms better?
- Has anyone else at home been ill?
- Is a sore throat a recurring problem?
- Do you smoke? Are you or your child regularly exposed to secondhand smoke?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



