End-stage renal disease
![]() November, 20th, 2024
November, 20th, 2024
Benefit Summary
When kidneys no longer function well enough to meet a body’s needs, treatment involves kidney dialysis or kidney transplant.
Overview
, Overview, ,
End-stage renal disease, also called end-stage kidney disease or kidney failure, occurs when chronic kidney disease — the gradual loss of kidney function — reaches an advanced state. In end-stage renal disease, your kidneys no longer work as they should to meet your body’s needs.
Your kidneys filter wastes and excess fluids from your blood, which are then excreted in your urine. When your kidneys lose their filtering abilities, dangerous levels of fluid, electrolytes and wastes can build up in your body.
With end-stage renal disease, you need dialysis or a kidney transplant to stay alive. But you can also choose to opt for conservative care to manage your symptoms — aiming for the best quality of life during your remaining time.
Symptoms
Early in chronic kidney disease, you might have no signs or symptoms. As chronic kidney disease progresses to end-stage renal disease, signs and symptoms might include:
- Nausea
- Vomiting
- Loss of appetite
- Fatigue and weakness
- Changes in how much you urinate
- Chest pain, if fluid builds up around the lining of the heart
- Shortness of breath, if fluid builds up in the lungs
- Swelling of feet and ankles
- High blood pressure (hypertension) that’s difficult to control
- Headaches
- Difficulty sleeping
- Decreased mental sharpness
- Muscle twitches and cramps
- Persistent itching
- Metallic taste
Signs and symptoms of kidney disease are often nonspecific, meaning they can also be caused by other illnesses. Because your kidneys can make up for lost function, signs and symptoms might not appear until irreversible damage has occurred.
When to seek care
Make an appointment with your health care provider if you have signs or symptoms of kidney disease.
If you have a medical condition that increases your risk of kidney disease, your care provider is likely to monitor your kidney function with urine and blood tests and your blood pressure during regular office visits. Ask your provider whether these tests are necessary for you.
Causes
Kidney disease occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years. For some people, kidney damage can continue to progress even after the underlying condition is resolved.
Diseases and conditions that can lead to kidney disease include:
- Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis) — an inflammation of the kidney’s filtering units (glomeruli)
- Interstitial nephritis (in-tur-STISH-ul nuh-FRY-tis), an inflammation of the kidney’s tubules and surrounding structures
- Polycystic kidney disease or other inherited kidney diseases
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis (pie-uh-low-nuh-FRY-tis)

A typical kidney has about 1 million filtering units. Each unit, called a glomerulus, joins a tubule. The tubule collects urine. Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring.

A healthy kidney (left) removes waste from the blood and maintains the body’s chemical balance. With polycystic kidney disease (right), fluid-filled sacs called cysts develop in the kidneys. The kidneys grow larger and slowly lose their ability to work as they should.
Polycystic kidney Risk factors
Certain factors increase the risk that chronic kidney disease will progress more quickly to end-stage renal disease, including:
- Diabetes with poor blood sugar control
- Kidney disease that affects the glomeruli, the structures in the kidneys that filter wastes from the blood
- Polycystic kidney disease
- High blood pressure
- Tobacco use
- Black, Hispanic, Asian, Pacific Islander or American Indian heritage
- Family history of kidney failure
- Older age
- Frequent use of medications that could be damaging to the kidney
Complications
Kidney damage, once it occurs, can’t be reversed. Potential complications can affect almost any part of your body and can include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart’s ability to function and may be life-threatening
- Heart disease
- Weak bones and an increased risk of bone fractures
- Anemia
- Decreased sex drive, erectile dysfunction or reduced fertility
- Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures
- Decreased immune response, which makes you more vulnerable to infection
- Pericarditis, an inflammation of the saclike membrane that envelops your heart (pericardium)
- Pregnancy complications that carry risks for the mother and the developing fetus
- Malnutrition
- Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival
Prevention
If you have kidney disease, you may be able to slow its progress by making healthy lifestyle choices:
- Achieve and maintain a healthy weight
- Be active most days
- Limit protein and eat a balanced diet of nutritious, low-sodium foods
- Control your blood pressure
- Take your medications as prescribed
- Have your cholesterol levels checked every year
- Control your blood sugar level
- Don’t smoke or use tobacco products
- Get regular checkups
Diagnosis
To diagnose end-stage renal disease, your health care provider may ask you about your family’s and your medical history. You may also have physical and neurological exams, along with other tests such as:
- Blood tests, to measure the amount of waste products, such as creatinine and urea, in your blood
- Urine tests, to check the level of the protein albumin in your urine
- Imaging tests, such as ultrasound, MRI or CT scan, to assess your kidneys and look for unusual areas
- Removing a sample of kidney tissue (biopsy), to examine under a microscope to learn what type of kidney disease you have and how much damage there is
Certain tests might be repeated over time to help your provider follow the progress of your kidney disease.
Stages of kidney disease
There are five stages of kidney disease. To determine what stage you have, your health care provider performs a blood test to check your glomerular filtration rate (GFR). The GFR measures how much blood the kidneys filter each minute, recorded as milliliters per minute (mL/min). As the GFR declines, so does your kidney function.
When your kidneys no longer work at a level that’s necessary to keep you alive, you have end-stage renal disease. End-stage renal disease usually occurs when kidney function is less than 15% of typical kidney function.
As a part of kidney disease staging, your provider also might test whether you have protein in your urine.
| Kidney disease stage | GFR, mL/min | Kidney function | |
|---|---|---|---|
| Source: National Kidney Foundation | |||
| Stage 1 | 90 or above | Healthy kidney function | |
| Stage 2 | 60 to 89 | Mild loss of kidney function | |
| Stage 3a | 45 to 59 | Mild to moderate loss of kidney function | |
| Stage 3b | 30 to 44 | Moderate to severe loss of kidney function | |
| Stage 4 | 15 to 29 | Severe loss of kidney function | |
| Stage 5 | Less than 15 | Kidney failure | |

During a kidney biopsy, your doctor uses a needle to remove a small sample of kidney tissue for lab testing. The biopsy needle is inserted through your skin and is often directed using the guidance of an imaging device, such as ultrasound.

During a kidney biopsy, your doctor uses a needle to remove a small sample of kidney tissue for lab testing. The biopsy needle is inserted through your skin and is often directed using the guidance of an imaging device, such as ultrasound.
Kidney biopsy Treatment
End-stage renal disease treatments include:
- Kidney transplant
- Dialysis
- Supportive care
Kidney transplant
A kidney transplant is a surgical procedure to place a healthy kidney from a live or deceased donor into a person whose kidneys no longer function properly. A kidney transplant is often the treatment of choice for end-stage renal disease, compared with a lifetime on dialysis.
The kidney transplant process takes time. It involves finding a donor, living or deceased, whose kidney best matches your own. You then have surgery to place the new kidney in your lower abdomen and attach the blood vessels and ureter — the tube that links the kidney to the bladder — that will allow the new kidney to function.
You may need to spend several days to a week in the hospital. After leaving the hospital, you can expect frequent checkups to monitor your progress as your recovery continues. You may take a number of medications to help keep your immune system from rejecting your new kidney and to reduce the risk of post-surgery complications, such as infection.
After a successful kidney transplant, your new kidney filters your blood, and you no longer need dialysis.
Dialysis
Dialysis does some of the work of your kidneys when your kidneys can’t do it themselves. This includes removing extra fluids and waste products from your blood, restoring electrolyte levels, and helping control your blood pressure.
Dialysis options include peritoneal dialysis and hemodialysis.
For dialysis to be successful, you may need to make lifestyle changes, such as following certain dietary recommendations.
Palliative care
If you choose not to have a kidney transplant or dialysis, you can choose palliative or supportive care to help you manage your symptoms and feel better. You also can combine palliative care with kidney transplant or dialysis.
Without either dialysis or a transplant, kidney failure progresses, eventually leading to death. Death can occur quickly or take months or years. Supportive care might include management of symptoms, measures to keep you comfortable and end-of-life planning.
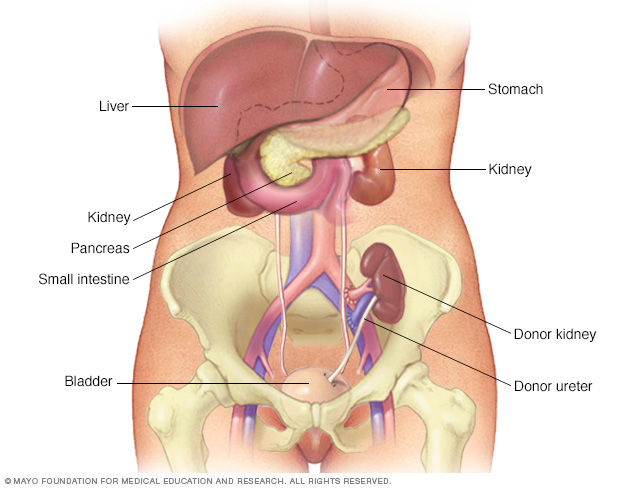
During kidney transplant surgery, the donor kidney is placed in your lower abdomen. Blood vessels of the new kidney are attached to blood vessels in the lower part of your abdomen, just above one of your legs. The new kidney’s urine tube (ureter) is connected to your bladder. Unless they are causing complications, your own kidneys are left in place.
Kidney transplant Lifestyle and home remedies
As part of your treatment for kidney disease, your health care provider might recommend that you follow a special diet to help support your kidneys and limit the work they must do. Ask for a referral to a registered dietitian with expertise in kidney disease to learn ways to make your diet easier on your kidneys.
Depending on your situation, kidney function and overall health, your dietitian might recommend that you:
- Avoid products with added salt. Lower the amount of sodium you eat each day by avoiding products with added salt, including many convenience foods, such as frozen dinners, canned soups and fast foods. Other foods with added salt include salty snack foods, canned vegetables, and processed meats and cheeses.
-
Choose lower potassium foods. Your dietitian might recommend that you choose lower potassium foods at each meal. High-potassium foods include bananas, oranges, potatoes, spinach and tomatoes.
Examples of low-potassium foods include apples, cabbage, carrots, green beans, grapes and strawberries. Be aware that many salt substitutes contain potassium, so you generally should avoid them if you have kidney failure.
- Limit your protein. Your dietitian will estimate the grams of protein you need each day and make recommendations based on that amount. High-protein foods include lean meats, eggs, milk, cheese and beans. Low-protein foods include vegetables, fruits, breads and cereals.
Coping and support
Learning you’re in kidney failure can come as a shock, even if you’ve known about your kidney disease for a while. It might be difficult to manage the treatment schedule if you’re on dialysis.
To help you cope, consider trying to:
- Connect with other people who have kidney disease. It might help you to talk to other people with end-stage renal disease Ask your doctor about support groups in your area. Or contact organizations such as the American Association of Kidney Patients, the National Kidney Foundation or the American Kidney Fund for groups in your area.
- Maintain your routine, when possible. Try to continue to work and do the activities you enjoy, if your condition allows.
- Be active most days of the week. With your provider’s approval, aim for at least 30 minutes of physical activity most days of the week. This can help you with fatigue and stress.
- Talk with someone you trust. It might help to talk about your feelings with a friend or family member, a faith leader, or someone else you trust. Your provider might be able to recommend a social worker or counselor.
Preparing for an appointment
For end-stage renal disease, you’ll likely continue to see the same health care provider and care team you’ve been seeing for treatment of chronic kidney disease. If you’re not already being cared for by a doctor who specializes in kidney problems (nephrologist), you might be referred to one as your disease progresses.
What you can do
To get ready for your appointment, ask if there’s anything you need to do ahead of time, such as make changes to your diet. Then take note of:
- Your symptoms, including any that seem unrelated to your kidneys or urinary function, and when thy began
- All your medications and doses, vitamins or other supplements you take
- Your key medical history, including other medical conditions and family history of kidney disease
- Questions to ask your provider
Take a family member or friend along, if possible, to help you remember the information you’re given.
For end-stage renal disease, some basic questions to ask your provider include:
- What’s the level of damage to my kidneys?
- Is my kidney function worsening?
- Do I need more tests?
- What’s causing my condition?
- Can the damage to my kidneys be reversed?
- What are my treatment options?
- What are the potential side effects of each treatment?
- I have these other health conditions. How can I best manage them together?
- Do I need to eat a special diet?
- Can you refer me to a dietitian who can help me plan my meals?
- Are there brochures or other printed material I can have? What websites do you recommend?
- How often do I need to have my kidney function tested?
Don’t hesitate to ask any other questions you have.
What to expect from your health care provider
Your provider may ask you questions, such as:
- Have you noticed changes in your urinary habits or unusual fatigue?
- Have you been diagnosed or treated for high blood pressure?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



