Prostatitis
![]() February, 26th, 2025
February, 26th, 2025
Benefit Summary
Learn about tests and treatments for conditions of the prostate gland that cause pain, trouble with urination, and other symptoms.
Overview
, Overview, ,
Prostatitis is a condition of the prostate gland most often linked with swelling and irritation, called inflammation. Prostatitis can make it painful or hard to urinate. It also may cause pain in the groin, pelvic area or genitals. Bacterial infections cause some but not all prostatitis.
The prostate gland, about the size of a walnut, sits just below the bladder in people assigned male at birth. It surrounds the top part of the tube that drains urine from the bladder, called the urethra. The prostate and other sex glands make the fluid that carries sperm during ejaculation. This fluid is called semen.
Types
There are four main types of prostatitis:
- Acute bacterial prostatitis. Bacteria causes this infection of the prostate. It most often has sudden, serious symptoms.
- Chronic bacterial prostatitis. This is a bacterial infection that lasts or comes back. The symptoms often are less serious than are those of acute bacterial prostatitis.
- Chronic prostatitis, also called chronic pelvic pain syndrome. This causes pelvic pain and urinary tract symptoms that last or come back. But there’s no sign of infection.
- Asymptomatic inflammatory prostatitis. This has signs of an inflamed prostate with no urinary symptoms.
Symptoms
Symptoms of prostatitis depend on the type of condition. They may include:
- Pain or burning feeling when urinating, called dysuria.
- Trouble urinating, such as dribbling or trouble starting a stream of urine or keeping it going.
- Urinating often, mostly at night, called nocturia.
- Urgent need to urinate.
- Cloudy urine.
- Blood in the urine.
- Pain in the belly, groin or lower back.
- Pain in the area between the scrotum and rectum, called the perineum.
- Pain or discomfort of the penis or testicles.
- Painful ejaculation.
- Fever, chills, muscle aches and other flu-like symptoms with acute bacterial prostatitis.
When to see a doctor
Several conditions can cause symptoms like those of prostatitis. Get a diagnosis and treatment as soon as possible.
Get care right away if you:
- Are not able to pass urine.
- Have a fever and trouble urinating or pain while urinating.
- Have blood in your urine.
- Have a lot of discomfort or pain in the pelvic area or genitals.
Causes
Causes depend on the type of prostatitis.
- Acute bacterial prostatitis. Common strains of bacteria are most often the cause. The infection may have spread from other parts of the urinary or reproductive systems.
- Chronic bacterial prostatitis. This most often has the same cause as acute bacterial infection. It may happen when treatment for an acute infection isn’t long enough or fails to kill all the bacteria.
- Chronic prostatitis, also called chronic pelvic pain syndrome. Research suggests that the cause may involve several factors. These include an earlier infection, a condition of the nervous system or immune system, psychological stress, or issues with hormones.
- Asymptomatic inflammatory prostatitis. This has no known cause. It may show up during an exam for other medical conditions.

The prostate gland sits just below the bladder. It surrounds the top part of the tube that drains urine from the bladder, called the urethra. The prostate’s main job is to make the fluid that feeds and carries sperm, called seminal fluid. The prostate is part of the male reproductive system.
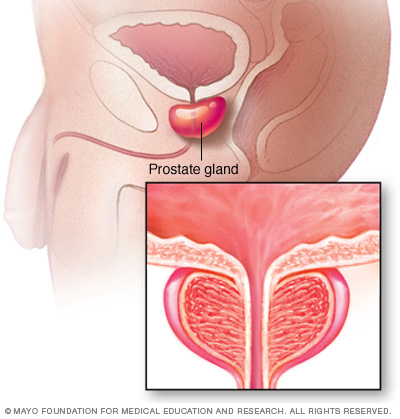
The prostate gland sits just below the bladder. It surrounds the top part of the tube that drains urine from the bladder, called the urethra. The prostate’s main job is to make the fluid that feeds and carries sperm, called seminal fluid. The prostate is part of the male reproductive system.
Prostate gland Risk factors
Risk factors for prostatitis include:
- Young or middle adulthood.
- Earlier prostatitis.
- Infection of the urinary or reproductive system.
- HIV infection or AIDS.
- Use of a tube put into the urethra to drain the bladder, called a urinary catheter.
- Having a sample of prostate tissue taken for study in a lab, called a biopsy.
Other risk factors for chronic prostatitis, also called chronic pelvic pain syndrome, may include:
- Mental stress.
- Nerve damage in the pelvic region due to surgery or injury.
Complications
Complications of acute or chronic prostatitis can include:
- Bacterial infection of the blood, called bacteremia.
- Irritation of the coiled tube attached to the back of the testicle, called epididymitis.
- Pus-filled cavity in the prostate, called a prostatic abscess.
- Infection that spreads to the upper pelvic bone or lower spine.
Complications of chronic prostatitis/chronic pelvic pain syndrome may include:
- Worry or depression.
- Sexual dysfunction, such as not being able get and keep an erection, called erectile dysfunction.
- Changes in sperm and semen that may affect having children, called infertility.
There’s no proof that prostatitis can lead to prostate cancer. Researchers are looking into whether long-term irritation of the prostate is a risk factor for cancer.
Diagnosis
Several conditions can cause symptoms like those of prostatitis. Your healthcare professional may send you to a specialist in urinary and reproductive system conditions, called a urologist. Diagnosis involves a physical exam, review of your symptoms and medical history, and tests.
Test for diagnosing bacterial infections
Diagnostic tests to assess for infection may include:
- Digital rectal exam. With this procedure, a healthcare professional puts a gloved finger that’s oiled into your rectum to see if there’s inflammation of the prostate.
- Urine test. A urine sample is tested for infection and what type it is.
- Blood test. Blood samples may show signs of infection and other prostate conditions.
- Prostatic specimen test. Sometimes, a healthcare professional gently massages the prostate during a rectal exam. This is to release prostate fluid into the urethra. A urine sample collected after the massage is tested to check for infection in the prostate fluid. This test is not for acute bacterial prostatitis because it can spread germs in the blood.
Other tests
If the first tests show no sign of infection, you may have other tests, including:
- Urodynamic tests. These tests measure how well the bladder and urethra hold and release urine. These tests can help show the source of issues with urinating.
- Imaging. Imaging tests can show something that isn’t usual in the prostate and growths or other issues in the pelvic region that may be causing pain.
Treatment
Treatment for prostatitis depends on the type you have and your symptoms.
Treating infection
For acute or chronic bacterial prostatitis, you take antibiotics. Acute prostatitis may need antibiotics given through a tube in a vein, called an IV, in the hospital for a short time.
The course of antibiotic treatment is most often 4 to 6 weeks. Sometimes it can be longer. Take all the medicine to get rid of the infection and lower the risk of chronic bacterial prostatitis.
Treating urinary symptoms
Medicines called alpha-blockers help relax the bladder neck and the muscle fibers where the prostate joins the bladder. This treatment might ease symptoms, such as pain while urinating or trouble urinating.
Alpha-blockers most often treat people with chronic prostatitis, also called chronic pelvic pain syndrome. Alpha-blockers also can ease urinary symptoms of bacterial infections.
Treating pain
Your healthcare professional may prescribe pain medicine or suggest medicines you can get without a prescription. These include acetaminophen (Tylenol, others) and ibuprofen (Advil, Motrin IB, others).
Managing psychological symptoms
Your healthcare professional may advise that you see a mental healthcare professional. This can help you manage stress, depression or worry that may be linked with long-term pain.
Lifestyle and home remedies
Do the following to help ease some symptoms of prostatitis:
- Soak in a warm bath, called a sitz bath, or use a heating pad.
- Don’t have or limit alcohol, caffeine, and spicy or high-acid foods. They can irritate the bladder.
- Drink plenty of water. This will make you urinate more and help flush bacteria from your bladder.
Alternative medicine
Alternative therapies that show some promise for easing symptoms of prostatitis include:
- Biofeedback. You use this mind-body technique to help you control some of your body’s work, such as heart rate and muscle responses. During biofeedback, you’re connected to electrical pads that help you learn how your body responds.
- Acupuncture. This treatment involves putting very thin needles through your skin at certain points on your body. Acupuncture may help ease pain.
- Herbal treatments. Some studies suggest that rye grass pollen extract, also called cernilton, may help manage the pain of chronic prostatitis, also called chronic pelvic pain syndrome. There isn’t enough proof that other herbal treatments ease symptoms of prostatitis.
Talk about your use of alternative medicine practices and herbal treatments with your healthcare professional before trying any.
Preparing for an appointment
Your healthcare professional will review your symptoms and medical history with you. Be ready to answer the following questions:
- When did your symptoms begin?
- Are your symptoms constant, or do they come and go?
- Do you have pain? Where?
- Do you have pain when urinating?
- Do you have trouble urinating, such as dribbling, or trouble starting a stream of urine or keeping it going?
- Have you seen bloody or cloudy urine?
- Have you had sudden, urgent needs to urinate?
- Are you urinating more often than usual?
- How often do you need to urinate in the night?
- Do you have pain when ejaculating?
- Have you been diagnosed with bacterial prostatitis or a urinary tract infection in the past? When?
- Did you take all the pills for that infection?
- Have you had a recent injury to your groin?
- What medicines, dietary supplements, herbal products and vitamins do you take?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



