Placenta previa
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Learn about how this pregnancy complication is diagnosed and managed to reduce risks to your baby’s health and your own.
Overview
, Overview, ,
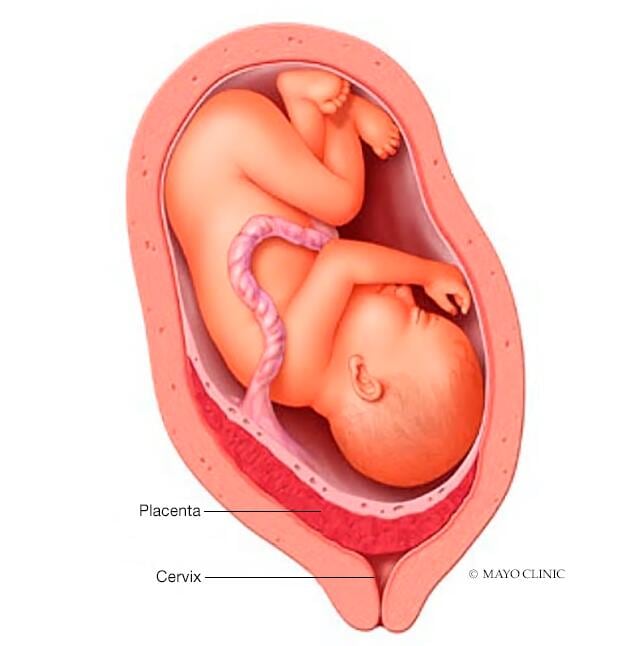
Placenta previa (pluh-SEN-tuh PREH-vee-uh) is a problem during pregnancy when the placenta completely or partially covers the opening of the uterus (cervix).
The placenta is an organ that develops inside the uterus during pregnancy. It works to provide oxygen and nutrition to the baby and to remove waste. The placenta connects to your baby through the umbilical cord. Typically, the placenta is attached to the top or side of the inner wall of the uterus.
With placenta previa, the placenta attaches lower in the uterus. This results in some portion of the placental tissue covering the cervix. It can result in bleeding during the pregnancy or during or after delivery.
Changes in the uterus and placenta during pregnancy may lead to the problem correcting on its own. If it doesn’t, the baby is delivered by cesarean section (C-section).
The main sign of placenta previa is bright red vaginal bleeding, usually without pain, after 20 weeks of pregnancy. Sometimes, spotting happens before an event with more blood loss.
The bleeding may occur with prelabor contractions of the uterus that cause pain. The bleeding may also be triggered by sex or during a medical exam. For some women, bleeding may not occur until labor. Often there is no clear event that leads to bleeding.
When to see a doctor
If you have vaginal bleeding during your second or third trimester, call your health care provider right away. If the bleeding is severe, seek emergency medical care.
Causes
The exact cause of placenta previa is unknown.
Risk factors
Placenta previa is more common among women who:
- Have had a baby
- Have had a previous C-section delivery
- Have scars on the uterus from a previous surgery or procedure
- Had placenta previa with a previous pregnancy
- Are pregnant after having an assisted reproductive technology (ART) procedure for treating infertility
- Are carrying more than one fetus
- Are age 35 or older
- Smoke
- Use cocaine
Complications
If you have placenta previa, your health care provider will monitor you and your baby to reduce the risk of these serious complications:
- Bleeding. Severe, possibly life-threatening vaginal bleeding (hemorrhage) can occur during the pregnancy, labor, delivery or in the first few hours after delivery.
- Preterm birth. Severe bleeding may prompt an emergency C-section before your baby is full term.
- Placenta accreta spectrum. Placenta previa is associated with a group of conditions called placenta accreta spectrum. With these conditions, the placenta grows into or through the wall of the uterus. Placenta accreta has a high risk of bleeding during pregnancy or during and after delivery.
Diagnosis
Placenta previa is diagnosed through ultrasound, either during a routine prenatal appointment or after an episode of vaginal bleeding. Most cases of placenta previa are diagnosed during a second-trimester ultrasound exam.
The initial diagnosis may be done with an ultrasound device on your abdomen. For more accurate images, you may also need a transvaginal ultrasound, which uses a wandlike device placed inside your vagina. Your provider will take care with the position of the device so as not to disrupt the placenta or cause bleeding.
Treatment
If placenta previa is diagnosed during a routine exam, you’ll likely have more-frequent ultrasound exams to monitor any changes in the placenta.
In many women diagnosed with placenta previa early in their pregnancies, the condition resolves on its own. As the uterus grows, the distance between the cervix and the placenta may increase. Also, the direction of growth of the placenta may be higher in the uterus, and the edges of placental tissue near the cervix may shrink.
If placenta previa resolves, you may be able to plan for a vaginal delivery. If it doesn’t resolve, you’ll plan for a C-section delivery.
Treatment of bleeding
Vaginal bleeding after 20 weeks is treated as a medical emergency. You may be admitted to the hospital’s labor and delivery unit. You and your baby will be monitored, and you may need a blood transfusion to replace lost blood.
If you are at 36 weeks, you’ll likely have a C-section to deliver the baby. If you have extreme blood loss or there’s a risk to the health of you or the baby, an emergency C-section may be needed before 36 weeks.
If this was the first time you’ve had bleeding and the bleeding has stopped for at least 48 hours, you may be sent home from the hospital. If you continue to have episodes of heavier bleeding, your health care team may recommend that you remain in the hospital.
Treatment with no bleeding
When there’s no bleeding, the treatment goal is to lower the risk of possible bleeding and to get you as close to your delivery date as possible. Your care provider will likely recommend you avoid the following:
- Sexual intercourse or sexual activity that could lead to orgasm
- Moderate or strenuous exercise
- Moderate or heavy lifting
- Standing for long periods of time
If you are sent home from the hospital after a first bleeding episode, you’ll be expected to follow these same recommendations to lower the risk of a second episode.
You’ll be advised to get emergency medical care if you have vaginal bleeding or contractions. Your health care provider may ask whether you have support at home that allows for transportation to a nearby hospital.
Planned C-section delivery
Even if you’ve had no bleeding during your pregnancy due to placenta previa — or no bleeding since the first episode — you’ll likely have a C-section delivery scheduled sometime between 36 and 37 weeks.
If your delivery is planned before 37 weeks, your health care provider will offer you corticosteroids to help your baby’s lungs develop.
Coping and support
If you’re diagnosed with placenta previa, you may worry about how your condition will affect you, your baby and your family. Some of these strategies might help you cope:
- Learn as much as you can about the condition.
- Find a support group through your clinic, hospital or other community organizations.
- Identify people who can help with daily activities at home or provide emotional support.
- Be specific about ways people can help if they offer you assistance.
- Make a transportation or child-care plan in case you need emergency services.
Preparing for your appointment
Placenta previa is usually diagnosed during a routine ultrasound exam or after an episode of vaginal bleeding. So you might not have time to prepare for an appointment about placenta previa as you might for typical prenatal care appointments.
If you don’t need immediate medical care or are being sent home after treatment for vaginal bleeding, it’s important to understand the plan for ongoing care and management.
Questions you may want to ask your provider after a diagnosis or at follow-up exams include:
- What signs or symptoms should prompt me to call you?
- What signs or symptoms should cause me to go to the hospital?
- When will I need my next ultrasound exam?
- What other follow-up care will I need?
- What activities do I need to stop or limit?
- What type of exercise do you recommend?
- Is there a possibility the placenta previa will resolve on its own?
- At what time will we likely know whether I can have a vaginal delivery?
- If we need to plan for a C-section delivery, when do you recommend scheduling it?
- Do you have additional information about placenta previa?
- Do you have information about support groups or services for women with placenta previa?
What to expect from your doctor
Your health care provider is likely to ask you a number of questions, regarding your ability to manage care at home, particularly if you’ve already had one bleeding episode. These include:
- How far do you live from the hospital?
- How long would it take to get to the hospital in an emergency, including time to arrange child care and transportation?
- Do you have someone who could care for you or help with daily activities, so that you can restrict your activities or rest?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



