Aortic valve stenosis
![]() January, 28th, 2025
January, 28th, 2025
Benefit Summary
This type of heart valve disease reduces or blocks blood flow from the heart to the body. Know the symptoms and how it’s treated.
Overview
, Overview, ,
Aortic valve stenosis is a type of heart valve disease, also called valvular heart disease. The aortic valve is between the lower left heart chamber and the body’s main artery, called the aorta. In aortic valve stenosis, the valve is narrowed and doesn’t open fully. This reduces or blocks blood flow from the heart to the aorta and to the rest of the body.
Treatment of aortic stenosis depends on how severe the condition is. Treatment may include surgery to fix or replace the valve. Without treatment, severe aortic valve stenosis can lead to life-threatening complications.
Symptoms
Aortic valve stenosis ranges from mild to severe. Symptoms generally happen when the valve is very narrowed. Some people with aortic valve stenosis may not have symptoms for many years.
Symptoms of aortic valve stenosis may include:
- Chest pain or tightness with activity.
- Feeling faint or dizzy or fainting with activity.
- Shortness of breath, especially with activity.
- Fatigue, especially during times of increased activity.
- Rapid, fluttering heartbeat.
Children with aortic valve stenosis may have other symptoms such as:
- Not eating enough.
- Not gaining enough weight.
Aortic valve stenosis may lead to heart failure. Heart failure symptoms include extreme tiredness, shortness of breath, and swollen ankles and feet.
When to see a doctor
If you have an irregular heartbeat or other symptoms of aortic valve stenosis, make an appointment with your healthcare professional.
Causes
To understand the causes of aortic valve stenosis, it may help to know how the heart and heart valves typically work.
The heart has four valves that keep blood flowing in the correct way:
- Aortic valve.
- Mitral valve.
- Tricuspid valve.
- Pulmonary valve.
Each valve has flaps, also called cusps, that open and close once during each heartbeat. Sometimes, the valves don’t open or close properly. If a valve doesn’t fully open or close, blood flow is reduced or blocked.
In aortic valve stenosis, the valve between the lower left heart chamber, called the left ventricle, and the body’s main artery, called the aorta, is narrowed and doesn’t open completely. This narrowing is called stenosis.
When the aortic valve opening is narrowed, the heart must work harder to pump enough blood to the body. The extra work can cause the lower left heart chamber to get thick. Eventually the heart may become weak.
Aortic valve stenosis causes include:
- Heart condition present at birth, called a congenital heart defect. Some children are born with an aortic valve that has only two cusps instead of the usual three. If there are only two cusps, it’s called a bicuspid aortic valve. Rarely, an aortic valve may have one or four cusps.
- Calcium buildup on the valve, called aortic valve calcification. Calcium is a mineral found in the blood. As blood moves over the aortic valve, calcium can collect on the valve. The calcium deposits may never cause any problems. Aortic valve stenosis that’s related to increasing age and calcium deposit buildup usually doesn’t cause symptoms until age 70 or 80. But in some people — particularly those with changes in the aortic valve at birth — calcium deposits might cause the valve to narrow at a younger age.
- Rheumatic fever. This complication of untreated strep throat can damage the heart valves. It may cause scar tissue to form on the aortic valve. Scar tissue can narrow the aortic valve opening. It also may make a rough surface on which calcium deposits can collect.
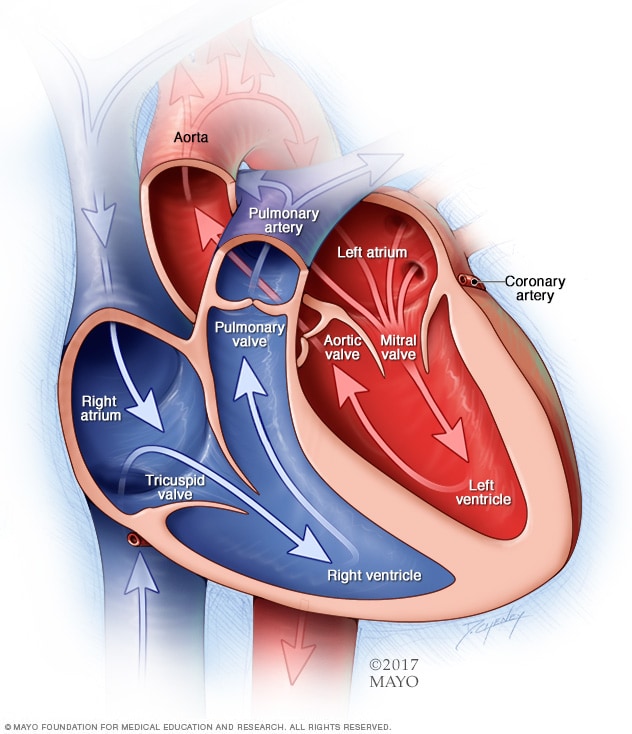
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves are gates at the chamber openings. They keep blood flowing in the right direction.

In aortic valve stenosis, the aortic valve opening is narrowed, as shown in the top image. The heart must work harder to pump blood across the smaller opening. This increases pressure within the heart. Eventually the strain reduces the heart’s ability to pump blood to the body. This is like placing smaller and smaller nozzles on the end of a garden hose, as shown on the bottom image. The narrower the nozzle is, the slower the flow of water. This results in pressure buildup within the garden hose.
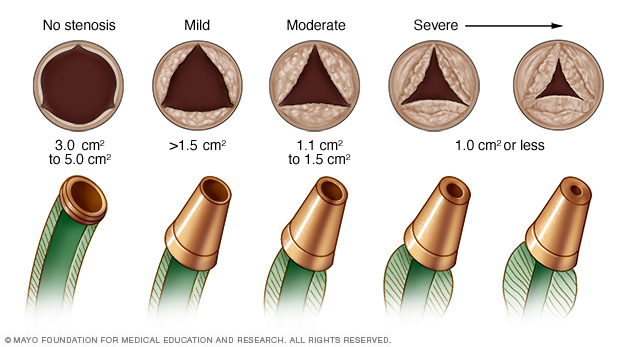
In aortic valve stenosis, the aortic valve opening is narrowed, as shown in the top image. The heart must work harder to pump blood across the smaller opening. This increases pressure within the heart. Eventually the strain reduces the heart’s ability to pump blood to the body. This is like placing smaller and smaller nozzles on the end of a garden hose, as shown on the bottom image. The narrower the nozzle is, the slower the flow of water. This results in pressure buildup within the garden hose.
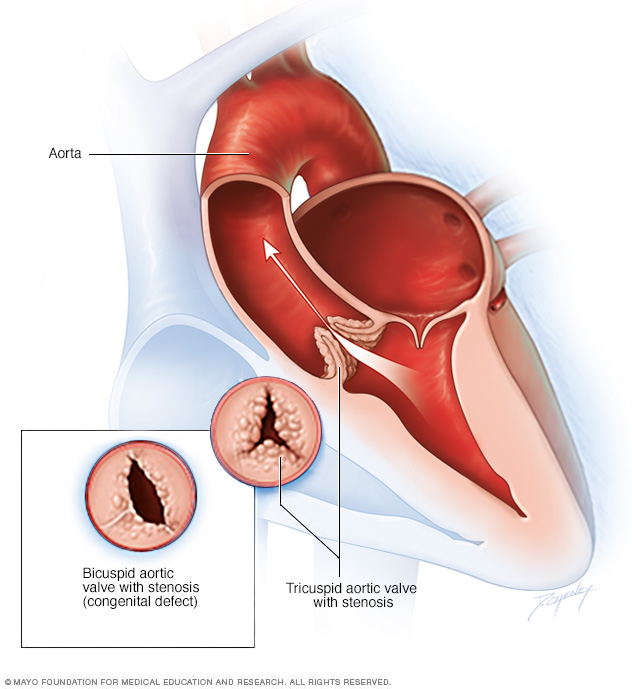
Aortic valve stenosis is a thickening and narrowing of the valve between the heart’s main pumping chamber and the body’s main artery, called the aorta. The narrowing creates a smaller opening for blood to pass through. This reduces or blocks blood flow from the heart to the rest of the body. Typically the aortic valve has three cusps, called a tricuspid aortic valve. But some people are born with an aortic valve that has two cusps, a condition called bicuspid aortic valve.
Aortic valve stenosis Risk factors
Risk factors of aortic valve stenosis include:
- Older age.
- Some heart conditions present at birth, called congenital heart defects. An example is a bicuspid aortic valve.
- Long-term kidney disease.
- Heart disease risk factors, such as diabetes, high cholesterol and high blood pressure.
- Infections that can affect the heart, such as rheumatic fever and infective endocarditis.
- Radiation therapy to the chest.
Complications
Possible complications of aortic valve stenosis are:
- Heart failure.
- Stroke.
- Blood clots.
- Bleeding.
- Irregular heartbeats, called arrhythmias.
- Infections that affect the heart, such as endocarditis.
Prevention
Some possible ways to prevent aortic valve stenosis are:
- Get a health checkup when you have a sore throat. Strep throat that is not treated can lead to rheumatic fever, which can damage heart valves. Strep throat can usually be easily treated with antibiotics. Rheumatic fever is more common in children and young adults.
- Keep the heart healthy. Talk about your risk factors for heart disease with your healthcare team. Ask how to prevent and manage them. Risk factors such as high blood pressure, obesity and high cholesterol may be linked to aortic valve stenosis.
- Take care of the teeth and gums. There may be a link between infected gums, called gingivitis, and a heart infection known as endocarditis. Endocarditis is a risk factor for aortic valve stenosis.
Diagnosis
To diagnose aortic valve stenosis, a healthcare professional examines you and asks questions about your symptoms and medical history. The health professional listens to your heart with a stethoscope. If you have aortic valve stenosis, a sound called a heart murmur may be heard.
Tests
Tests can tell if you have aortic valve stenosis. They also can learn the cause and how severe the condition is.
Tests for aortic valve stenosis may include:
-
Echocardiogram. Sound waves are used to make pictures of the beating heart. An echocardiogram shows how blood flows through the heart and heart valves. It can tell how severe aortic valve stenosis is. The test also can show if the heart muscle is weakened.
There are different types of echocardiograms. The type you have depends on the information your healthcare team needs. A standard echocardiogram is done from outside the body. An ultrasound device moves over the skin of the chest above the heart. If more details are needed about the heart, a transesophageal echocardiogram may be done. This type creates pictures of the heart from inside the body. The ultrasound device attaches to a tube that goes down the throat and into the esophagus.
- Electrocardiogram (ECG or EKG). This quick test records the electrical activity of the heart. It shows how the heart beats. Sticky patches with sensors on them go on the chest and sometimes the legs. Wires connect the patches to a computer, which displays or prints results. Your healthcare professional can look for signal patterns related to heart disease or swelling of the heart’s chambers.
- Chest X-ray. A chest X-ray shows the condition of the heart and lungs. It can show if the heart is bigger than usual, which can occur in aortic valve stenosis. It also can tell if there is calcium buildup on the aortic valve.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart’s activity is checked. Exercise tests show how the heart reacts to physical activity and whether valve disease symptoms happen during exercise. If you can’t exercise, you may get medicine that affects the heart like exercise does.
- Cardiac computerized tomography (CT) scan. This test uses several X-rays to create detailed images of the heart and heart valves. The test may be done to check the size of the aorta and look at the aortic valve more closely. A CT scan may be done to see how much calcium buildup is on the valve. It also can show how severe the aortic valve stenosis is.
- Cardiac magnetic resonance imaging (MRI) scan. A cardiac MRI uses magnetic fields and radio waves to create detailed images of the heart. This test can show the size of the aorta. It may be used to learn how severe the aortic valve stenosis is.
- Cardiac catheterization. This test isn’t often used to diagnose aortic valve disease. But it may be done to see how severe aortic valve disease is or to diagnose the condition if other tests can’t. In this test, a doctor places a thin, flexible tube into a blood vessel, usually in the groin area or arm, and guides it to the heart. Cardiac catheterization also may be used before aortic valve surgery to make sure the heart arteries are not blocked.
After testing confirms a diagnosis of aortic valve disease, your healthcare professional may tell you the stage of disease. Staging helps your healthcare team pick the most appropriate treatment.
Heart valve disease is staged into four basic groups:
- Stage A: At risk. Risk factors for heart valve disease are present.
- Stage B: Progressive. Valve disease is mild or moderate. There are no heart valve symptoms.
- Stage C: Asymptomatic severe. There are no heart valve symptoms but the valve disease is severe.
- Stage D: Symptomatic severe. Heart valve disease is severe and is causing symptoms.
The stage of heart valve disease depends on many things, including symptoms, disease severity, the structure of the valve or valves, and blood flow through the heart and lungs.
Treatment
Treatment for aortic valve stenosis depends on the symptoms and how severe the condition is. Aortic valve stenosis ranges from mild to severe.
If you have no symptoms or just mild ones, you may only need regular health checkups. Some people need medicines to treat valve disease symptoms or reduce the risk of complications.
Other treatments for aortic valve disease may include:
- Heart-healthy lifestyle changes. Eat healthy, get regular exercise and stay active, and do not smoke.
- Medicines to treat symptoms or reduce the risk of complications.
- Surgery to fix or replace the valve.
Medications
Some people with aortic valve stenosis may need medicines to treat symptoms or reduce the risk of complications. For example, medicines may be used to:
- Lower blood pressure.
- Prevent irregular heartbeats.
- Remove excess fluid from the body to reduce the strain on the heart.
Surgery or other procedures
You may eventually need a surgery to repair or replace the narrowed aortic valve, even if you don’t have symptoms. Aortic valve surgery may be done at the same time as other types of heart surgery.
Surgery to repair or replace an aortic valve is usually done through a cut in the chest. Less invasive approaches may be available. Ask your healthcare professional which type of aortic valve treatment is best for you.
Surgery and procedures for aortic valve stenosis include:
-
Balloon valvuloplasty. This treatment helps open a narrowed valve. It may be done in infants and children with aortic valve stenosis. In adults, the aortic valve tends to narrow again after the treatment. So it’s usually done only if an adult is too sick for surgery or if an adult is waiting for a valve replacement.
In balloon valvuloplasty, a doctor places a thin tube into a blood vessel in the arm or groin and guides it to the aortic valve. Once in place, a balloon on the tip of the tube is inflated. This makes the valve opening wider. The balloon is deflated. The tube and balloon are removed.
-
Aortic valve replacement. Aortic valve replacement is often needed to treat aortic valve stenosis. In aortic valve replacement, the surgeon takes out the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue. A tissue valve is called a biological tissue valve.
Sometimes, the aortic valve is replaced with the person’s own lung valve, called the pulmonary valve. The pulmonary valve is replaced with a biological lung tissue valve from a deceased donor. This more complicated surgery is called the Ross procedure.
Biological tissue valves break down over time and may eventually need to be replaced. People with mechanical valves need to take blood thinners for life to prevent blood clots. Talk with your healthcare team about the benefits and risks of each type of valve.
-
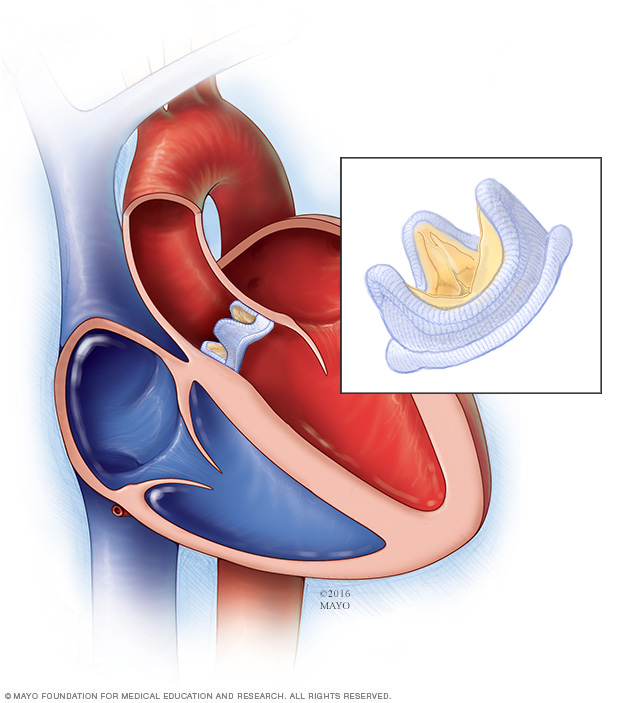
Transcatheter aortic valve replacement (TAVR). TAVR is an option to open-heart valve surgery. It uses small cuts and a thin, flexible tube called a catheter to replace the aortic valve. During TAVR, a surgeon replaces a narrowed aortic valve with a valve made of cow or pig tissue. TAVR may be an option if you’re at intermediate or high risk of complications from surgical aortic valve replacement. Ask your healthcare team about your options.
During TAVR, the surgeon places a tube into a blood vessel and guides it to the heart. A replacement valve made of cow or pig tissue goes through the tube to the aortic valve area. A balloon on the tube’s tip inflates to press the new valve into place. Some valves can self-expand. The tube is removed. Surgeons also may use tubes, called catheters, to put a replacement valve into a biological tissue valve that is no longer working properly.
- Aortic valve repair. Surgeons may fix the aortic valve by separating valve flaps that are stuck together. However, valve repair is rarely used to treat aortic valve stenosis. Generally aortic valve stenosis requires aortic valve replacement.
In a biological valve replacement, a valve made from cow, pig or human heart tissue replaces the damaged heart valve.
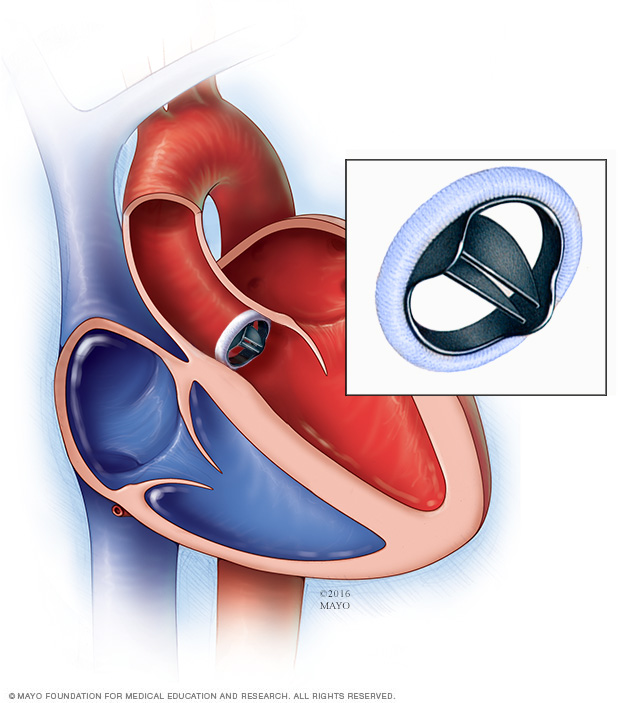
In a mechanical valve replacement, an artificial heart valve made of strong material replaces the damaged valve.
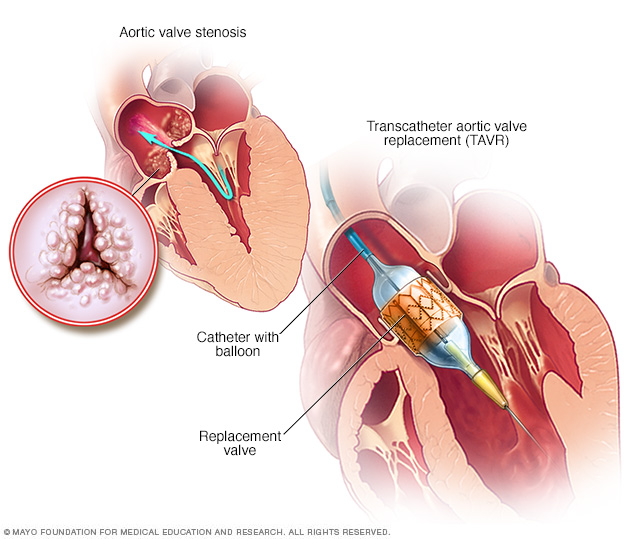
Transcatheter aortic valve replacement (TAVR) is a type of heart valve surgery. It’s done to replace a narrowed aortic valve, a condition called aortic valve stenosis. A doctor inserts a flexible tube called a catheter into a blood vessel and guides it into the heart. A replacement valve made of cow or pig tissue goes through the tube to the specific area in the heart. A balloon on the catheter tip inflates to press the new valve into place. Some valves are self-expanding.
Transcatheter aortic valve replacement (TAVR) Lifestyle and home remedies
Try these tips to help prevent or slow aortic valve stenosis and other types of heart disease.
- Do not smoke or use tobacco. Smoking is a major risk factor for heart disease. If you smoke and can’t quit, talk to your care team about programs or treatments that can help.
- Eat a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Limit salt and saturated fats.
- Keep a healthy weight. Lose weight if you are overweight or have obesity. Losing just a few pounds can help reduce risk factors for heart disease. Ask your healthcare professional what weight is best for you.
- Get regular exercise. Exercise helps manage weight and control risk factors for heart disease. Exercise at least 30 minutes a day on most days of the week. Talk with your healthcare team about the amount and type of exercise that’s best for you.
- Manage stress. Learn ways to help reduce emotional stress. Some ideas are to get more exercise, practice mindfulness or connect with others in support groups.
- Control blood pressure, blood sugar and cholesterol. Make lifestyle changes and take medicines as directed. Get regular health checkups.
- Limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Get good sleep. Poor sleep may increase the risk of heart disease and other health conditions. Adults should aim for 7 to 9 hours daily.
If you have aortic valve stenosis, your healthcare team may recommend that you limit strenuous activity to avoid overworking your heart.
Pregnancy and aortic valve disease
If you have aortic stenosis and are considering pregnancy, it’s important to talk with your healthcare team about your plans. Together, you can talk about the safety of medicines and whether you need treatment for aortic valve stenosis before getting pregnant.
Those with heart valve disease such as aortic valve stenosis usually require close checkups by a healthcare professional during pregnancy. If you have severe aortic stenosis, healthcare professionals may tell you not to get pregnant due to the risk of complications.
Preparing for an appointment
If you think you have aortic valve disease, make an appointment for a health checkup. Consider being seen and treated at a medical center with a multidisciplinary heart valve team. This is a team of heart doctors, called cardiologists, and other healthcare professionals trained and experienced in heart valve disease.
Here’s some information to help you prepare for your appointment.
What you can do
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there’s anything you need to do in advance. For example, you may be told not to eat or drink for a few hours before a cholesterol test.
- Write down your symptoms, including any that seem unrelated to aortic valve stenosis or the heart.
- Write down important personal information. Include any family history of heart disease and any major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you take. Include the dosages.
- Take someone with you, if possible. Someone who goes with you can help you remember information you receive.
- Write down questions to ask your healthcare professional.
For aortic valve stenosis, some basic questions to ask your healthcare professional are:
- What is the likely cause of my symptoms or condition?
- What are other possible causes?
- What tests do I need?
- What’s the best treatment?
- What are the options to the treatment you suggested?
- I have other health conditions. How can I best manage them together?
- How do I need to change my diet or activities?
- Should I see a specialist?
- If I need surgery, which surgeon do you recommend for heart valve surgery?
- Is there any information about my condition that I can take home with me? What websites do you recommend?
Don’t hesitate to ask any other questions.
What to expect from your doctor
Your healthcare team is likely to ask you many questions such as:
- When did your symptoms start?
- Do you always have symptoms, or do they come and go?
- How bad are your symptoms?
- What, if anything, makes your symptoms better?
- What, if anything, makes your symptoms worse?
- Does anyone in your family have heart disease?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



