Lupus
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Learn how this disease can affect your joints, skin, kidneys and other areas of your body, along with how to get symptom control.
Overview
, Overview, ,
Lupus is a disease that occurs when your body’s immune system attacks your own tissues and organs (autoimmune disease). Inflammation caused by lupus can affect many different body systems — including your joints, skin, kidneys, blood cells, brain, heart and lungs.
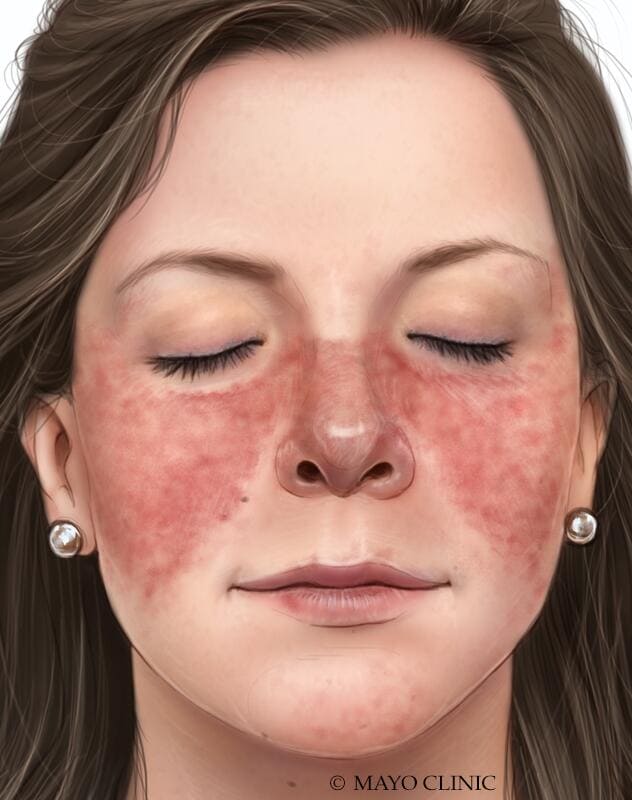
Lupus can be difficult to diagnose because its signs and symptoms often mimic those of other ailments. The most distinctive sign of lupus — a facial rash that resembles the wings of a butterfly unfolding across both cheeks — occurs in many but not all cases of lupus.
Some people are born with a tendency toward developing lupus, which may be triggered by infections, certain drugs or even sunlight. While there’s no cure for lupus, treatments can help control symptoms.
Symptoms
No two cases of lupus are exactly alike. Signs and symptoms may come on suddenly or develop slowly, may be mild or severe, and may be temporary or permanent. Most people with lupus have mild disease characterized by episodes — called flares — when signs and symptoms get worse for a while, then improve or even disappear completely for a time.
The signs and symptoms of lupus that you experience will depend on which body systems are affected by the disease. The most common signs and symptoms include:
- Fatigue
- Fever
- Joint pain, stiffness and swelling
- Butterfly-shaped rash on the face that covers the cheeks and bridge of the nose or rashes elsewhere on the body
- Skin lesions that appear or worsen with sun exposure
- Fingers and toes that turn white or blue when exposed to cold or during stressful periods
- Shortness of breath
- Chest pain
- Dry eyes
- Headaches, confusion and memory loss
See your doctor if you develop an unexplained rash, ongoing fever, persistent aching or fatigue.
Causes
As an autoimmune disease, lupus occurs when your immune system attacks healthy tissue in your body. It’s likely that lupus results from a combination of your genetics and your environment.
It appears that people with an inherited predisposition for lupus may develop the disease when they come into contact with something in the environment that can trigger lupus. The cause of lupus in most cases, however, is unknown. Some potential triggers include:
- Sunlight. Exposure to the sun may bring on lupus skin lesions or trigger an internal response in susceptible people.
- Infections. Having an infection can initiate lupus or cause a relapse in some people.
- Medications. Lupus can be triggered by certain types of blood pressure medications, anti-seizure medications and antibiotics. People who have drug-induced lupus usually get better when they stop taking the medication. Rarely, symptoms may persist even after the drug is stopped.
Risk factors
Factors that may increase your risk of lupus include:
- Your sex. Lupus is more common in women.
- Age. Although lupus affects people of all ages, it’s most often diagnosed between the ages of 15 and 45.
- Race. Lupus is more common in African Americans, Hispanics and Asian Americans.
Complications
Inflammation caused by lupus can affect many areas of your body, including your:
- Kidneys. Lupus can cause serious kidney damage, and kidney failure is one of the leading causes of death among people with lupus.
- Brain and central nervous system. If your brain is affected by lupus, you may experience headaches, dizziness, behavior changes, vision problems, and even strokes or seizures. Many people with lupus experience memory problems and may have difficulty expressing their thoughts.
- Blood and blood vessels. Lupus may lead to blood problems, including a reduced number of healthy red blood cells (anemia) and an increased risk of bleeding or blood clotting. It can also cause inflammation of the blood vessels.
- Lungs. Having lupus increases your chances of developing an inflammation of the chest cavity lining, which can make breathing painful. Bleeding into lungs and pneumonia also are possible.
- Heart. Lupus can cause inflammation of your heart muscle, your arteries or heart membrane. The risk of cardiovascular disease and heart attacks increases greatly as well.
Other types of complications
Having lupus also increases your risk of:
- Infection. People with lupus are more vulnerable to infection because both the disease and its treatments can weaken the immune system.
- Cancer. Having lupus appears to increase your risk of cancer; however, the risk is small.
- Bone tissue death. This occurs when the blood supply to a bone declines, often leading to tiny breaks in the bone and eventually to the bone’s collapse.
- Pregnancy complications. Women with lupus have an increased risk of miscarriage. Lupus increases the risk of high blood pressure during pregnancy and preterm birth. To reduce the risk of these complications, doctors often recommend delaying pregnancy until your disease has been under control for at least six months.
Diagnosis
Diagnosing lupus is difficult because signs and symptoms vary considerably from person to person. Signs and symptoms of lupus may change over time and overlap with those of many other disorders.
No one test can diagnose lupus. The combination of blood and urine tests, signs and symptoms, and physical examination findings leads to the diagnosis.
Laboratory tests
Blood and urine tests may include:
- Complete blood count. This test measures the number of red blood cells, white blood cells and platelets as well as the amount of hemoglobin, a protein in red blood cells. Results may indicate you have anemia, which commonly occurs in lupus. A low white blood cell or platelet count may occur in lupus as well.
- Erythrocyte sedimentation rate. This blood test determines the rate at which red blood cells settle to the bottom of a tube in an hour. A faster than normal rate may indicate a systemic disease, such as lupus. The sedimentation rate isn’t specific for any one disease. It may be elevated if you have lupus, an infection, another inflammatory condition or cancer.
- Kidney and liver assessment. Blood tests can assess how well your kidneys and liver are functioning. Lupus can affect these organs.
- Urinalysis. An examination of a sample of your urine may show an increased protein level or red blood cells in the urine, which may occur if lupus has affected your kidneys.
- Antinuclear antibody (ANA) test. A positive test for the presence of these antibodies — produced by your immune system — indicates a stimulated immune system. While most people with lupus have a positive ANA test, most people with a positive ANA do not have lupus. If you test positive for ANA , your doctor may advise more-specific antibody testing.
Imaging tests
If your doctor suspects that lupus is affecting your lungs or heart, he or she may suggest:
- Chest X-ray. An image of your chest may reveal abnormal shadows that suggest fluid or inflammation in your lungs.
- Echocardiogram. This test uses sound waves to produce real-time images of your beating heart. It can check for problems with your valves and other portions of your heart.
Biopsy
Lupus can harm your kidneys in many different ways, and treatments can vary, depending on the type of damage that occurs. In some cases, it’s necessary to test a small sample of kidney tissue to determine what the best treatment might be. The sample can be obtained with a needle or through a small incision.
Skin biopsy is sometimes performed to confirm a diagnosis of lupus affecting the skin.
Treatment
Treatment for lupus depends on your signs and symptoms. Determining whether you should be treated and what medications to use requires a careful discussion of the benefits and risks with your doctor.
As your signs and symptoms flare and subside, you and your doctor may find that you’ll need to change medications or dosages. The medications most commonly used to control lupus include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter NSAIDs, such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others), may be used to treat pain, swelling and fever associated with lupus. Stronger NSAIDs are available by prescription. Side effects of NSAIDs may include stomach bleeding, kidney problems and an increased risk of heart problems.
- Antimalarial drugs. Medications commonly used to treat malaria, such as hydroxychloroquine (Plaquenil), affect the immune system and can help decrease the risk of lupus flares. Side effects can include stomach upset and, very rarely, damage to the retina of the eye. Regular eye exams are recommended when taking these medications.
- Corticosteroids. Prednisone and other types of corticosteroids can counter the inflammation of lupus. High doses of steroids such as methylprednisolone (Medrol) are often used to control serious disease that involves the kidneys and brain. Side effects include weight gain, easy bruising, thinning bones, high blood pressure, diabetes and increased risk of infection. The risk of side effects increases with higher doses and longer term therapy.
- Immunosuppressants. Drugs that suppress the immune system may be helpful in serious cases of lupus. Examples include azathioprine (Imuran, Azasan), mycophenolate (Cellcept), methotrexate (Trexall, Xatmep, others), cyclosporine (Sandimmune, Neoral, Gengraf) and leflunomide (Arava). Potential side effects may include an increased risk of infection, liver damage, decreased fertility and an increased risk of cancer.
-
Biologics. A different type of medication, belimumab (Benlysta) administered intravenously, also reduces lupus symptoms in some people. Side effects include nausea, diarrhea and infections. Rarely, worsening of depression can occur.
Rituximab (Rituxan, Truxima) may be beneficial for some people in whom other medications haven’t helped. Side effects include allergic reaction to the intravenous infusion and infections.
In clinical trials, voclosporin has been shown to be effective in treating lupus.
Other potential drugs to treat lupus are currently being studied, including abatacept (Orencia), anifrolumab and others.
Self care
Take steps to care for your body if you have lupus. Simple measures can help you prevent lupus flares and, should they occur, better cope with the signs and symptoms you experience. Try to:
- See your doctor regularly. Having regular checkups instead of only seeing your doctor when your symptoms worsen may help your doctor prevent flares, and can be useful in addressing routine health concerns, such as stress, diet and exercise that can be helpful in preventing lupus complications.
- Be sun smart. Because ultraviolet light can trigger a flare, wear protective clothing — such as a hat, long-sleeved shirt and long pants — and use sunscreen with a sun protection factor (SPF) of at least 55 every time you go outside.
- Get regular exercise. Exercise can help keep your bones strong, reduce your risk of heart attack and promote general well-being.
- Don’t smoke. Smoking increases your risk of cardiovascular disease and can worsen the effects of lupus on your heart and blood vessels.
- Eat a healthy diet. A healthy diet emphasizes fruits, vegetables and whole grains. Sometimes you may have dietary restrictions, especially if you have high blood pressure, kidney damage or gastrointestinal problems.
- Ask your doctor if you need vitamin D and calcium supplements. There is some evidence to suggest that people with lupus may benefit from supplemental vitamin D. A calcium supplement can help you meet the daily recommended dietary allowance of 1,000 milligrams to 1,200 milligrams — depending on your age — to help keep your bones healthy.
Alternative medicine
Sometimes people with lupus seek alternative or complementary medicine. There aren’t any alternative therapies that have been shown to alter the course of lupus, although some may help ease symptoms of the disease.
Discuss these treatments with your doctor before initiating them on your own. He or she can help you weigh the benefits and risks and tell you if the treatments will interfere adversely with your current lupus medications.
Complementary and alternative treatments for lupus include:
- Dehydroepiandrosterone (DHEA). Taking supplements containing this hormone along with conventional treatment may help reduce lupus flares. DHEA may lead to acne in women.
- Fish oil. Fish oil supplements contain omega-3 fatty acids that may be beneficial for people with lupus. Preliminary studies have found some promise, though more study is needed. Side effects of fish oil supplements can include nausea, belching and a fishy taste in the mouth.
- Acupuncture. This therapy uses tiny needles inserted just under the skin. It may help ease the muscle pain associated with lupus.
Coping and support
If you have lupus, you’re likely to have a range of painful feelings about your condition, from fear to extreme frustration. The challenges of living with lupus increase your risk of depression and related mental health problems, such as anxiety, stress and low self-esteem. To help you cope, try to:
- Learn all you can about lupus. Write down any questions you have about lupus as they occur to you so that you can ask them at your next appointment. Ask your doctor or nurse for reputable sources of further information. The more you know about lupus, the more confident you’ll feel in your treatment choices.
-
Gather support among your friends and family. Talk about lupus with your friends and family and explain ways they can help out when you’re having flares. Lupus can be frustrating for your loved ones because they usually can’t see it, and you may not appear sick.
Family and friends can’t tell if you’re having a good day or a bad day unless you tell them. Be open about what you’re feeling so that your loved ones know what to expect.
- Take time for yourself. Cope with stress in your life by taking time for yourself. Use that time to read, meditate, listen to music or write in a journal. Find activities that calm and renew you.
- Connect with others who have lupus. Talk to other people who have lupus. You can connect through support groups in your community or through online message boards. Other people with lupus can offer unique support because they’re facing many of the same obstacles and frustrations that you’re facing.
Preparing for your appointment
You’re likely to start by seeing your primary care doctor, but he or she may refer you to a specialist in the diagnosis and treatment of inflammatory joint conditions and immune disorders (rheumatologist).
Because the symptoms of lupus can mimic so many other health problems, you may need patience while waiting for a diagnosis. Your doctor must rule out a number of other illnesses before diagnosing lupus. You may need to see a number of specialists such as doctors who treat kidney problems (nephrologists), blood disorders (hematologists) or nervous system disorders (neurologists) depending on your symptoms, to help with diagnosis and treatment.
What you can do
Before your appointment, you may want to write a list of answers to the following questions:
- When did your symptoms begin? Do they come and go?
- Does anything seem to trigger your symptoms?
- Have your parents or siblings had lupus or other autoimmune disorders?
- What medications and supplements do you take regularly?
You may also want to write down questions to ask your doctor, such as:
- What are the possible causes of my symptoms or condition?
- What tests do you recommend?
- If these tests don’t pinpoint the cause of my symptoms, what additional tests might I need?
- Are there any treatments or lifestyle changes that might help my symptoms now?
- Do I need to follow any restrictions while we’re seeking a diagnosis?
- Should I see a specialist?
- If you are considering pregnancy, be sure to discuss this with your doctor. Some medications cannot be used if you get pregnant.
In addition to the questions that you’ve prepared to ask your doctor, don’t hesitate to ask questions during your appointment at any time that you don’t understand something.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may leave time to go over any points you want to spend more time on. Your doctor may ask:
- Does sun exposure cause you to develop skin rashes?
- Do your fingers become pale, numb or uncomfortable in the cold?
- Do your symptoms include any problems with memory or concentration?
- How much do your symptoms limit your ability to function at school, at work or in personal relationships?
- Have you been diagnosed with any other medical conditions?
- Are you pregnant, or do you plan to become pregnant?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



