Polyhydramnios
![]() September, 25th, 2024
September, 25th, 2024
Benefit Summary
Learn about the symptoms, causes and treatment for this condition, in which too much amniotic fluid builds up during pregnancy.
Overview
, Overview, ,
Polyhydramnios (pol-e-hi-DRAM-nee-os) is the buildup of increased amniotic fluid — the fluid that surrounds the baby in the uterus during pregnancy. Polyhydramnios happens in about 1% to 2% of pregnancies.
Most of the time, the condition is mild. It’s often found during the middle or later stages of pregnancy. Severe polyhydramnios may cause shortness of breath, preterm labor or other symptoms.
If you learn that you have polyhydramnios, your health care team carefully tracks your pregnancy to help prevent health problems. Treatment depends on how serious the condition is. Mild polyhydramnios may go away on its own. Severe polyhydramnios may need to be watched more closely by your care team.
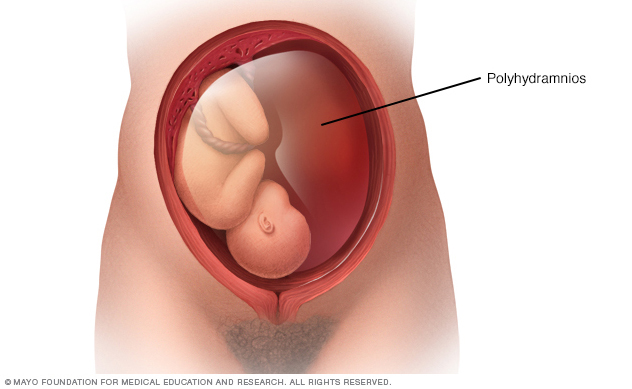
In polyhydramnios, increased levels of amniotic fluid accumulates in the uterus during pregnancy. Mild cases of polyhydramnios may go away on their own. Severe cases may require treatment.
Polyhydramnios during pregnancy Symptoms
Polyhydramnios symptoms may be linked with the buildup of amniotic fluid creating pressure within the uterus and on nearby organs. Mild polyhydramnios often causes few or no symptoms. But serious forms of the condition may cause:
- Shortness of breath or not being able to breathe.
- Swelling in the ankles or feet.
- Pain in the stomach area.
- Feelings of tightness in the muscles of the uterus, called contractions.
Your health care professional also may also suspect polyhydramnios if your uterus has become large for the number of weeks of pregnancy.
Causes
Some of the known causes of polyhydramnios include:
- Conditions that affect the baby’s digestive tract, central nervous system or certain other organs.
- Genetic conditions that affect the baby.
- Diabetes in the pregnant person.
- A complication of identical twin pregnancies in which one twin receives too much blood and the other too little. This is called twin-to-twin transfusion syndrome.
- A decreased amount of red blood cells in the baby, also called fetal anemia.
- A condition in which the pregnant parent’s blood cells attack the baby’s blood cells.
- Infection during pregnancy.
Often, the cause of polyhydramnios isn’t clear, especially when the condition is mild.
Risk factors
Risk factors for polyhydramnios include certain conditions that develop during pregnancy, such as gestational diabetes. A condition that affects the developing baby, such as a problem with the digestive tract, central nervous system or other organs, may also put you at risk of polyhydramnios.
Complications
Polyhydramnios is linked with:
- The baby being born too early, also called premature birth.
- The baby not being head-down in the ideal position before delivery, also called a breech birth.
- The water breaking early, also called premature rupture of membranes.
- The baby’s umbilical cord dropping into the vagina ahead of the baby, also called umbilical cord prolapse.
- The organ that provides oxygen and nutrients to the unborn baby, the placenta, peeling away from the inner wall of the uterus before delivery. This is called placental abruption.
- Need for a C-section delivery.
- Pregnancy loss after 20 weeks, also called stillbirth.
- Heavy bleeding due to decreased uterine muscle tone after delivery.
Greater health problems usually are linked with severe polyhydramnios.
Diagnosis
To find out if you have polyhydramnios, you’ll likely have a fetal ultrasound. This test uses high-frequency sound waves to make images of your unborn baby on a monitor.
Health care professionals can check for polyhydramnios by measuring the single largest pocket of amniotic fluid around the baby. This is called the maximum vertical pocket (MVP). Or they might measure the fluid in the four quadrants of the uterus, also called the amniotic fluid index (AFI). Polyhydramnios is diagnosed if the MVP is 8 or greater, or the AFI is 24 or greater.
Depending on the timing and how serious polyhydramnios is, your health care team may recommend other tests to try to determine the cause of the polyhydramnios:
- Blood tests. These can check for infectious diseases linked with polyhydramnios.
- Amniocentesis. This is a procedure in which a sample of amniotic fluid is removed from the uterus for testing. The fluid contains fetal cells and various chemicals produced by the baby. The cells in the fluid also can be used for genetic testing if there is concern for a genetic disorder.
Your health care team closely tracks your pregnancy if you have polyhydramnios. You may receive the following exams:
- Nonstress test. This test checks how your baby’s heart rate reacts when your baby moves. During the test, you’ll wear a special device on your stomach, also called the abdomen, to measure the baby’s heart rate. A buzzer-like device also may be used to wake the baby and encourage movement.
- Biophysical profile. This test uses an ultrasound to provide more information about your baby’s breathing, tone and movement. It also can help measure the volume of amniotic fluid in the uterus. It may be combined with a nonstress test.
Treatment
Mild polyhydramnios rarely needs treatment. It may go away on its own.
Otherwise, treatment for an underlying cause — such as diabetes — may help clear up polyhydramnios.
You may need treatment in the hospital if you have severe polyhydramnios with symptoms such as shortness of breath, stomach pain or contractions. Polyhydramnios treatment may include:
- Drainage of extra amniotic fluid. Your health care team may use amniocentesis to drain the extra amniotic fluid from your uterus. This procedure carries a small risk of health problems. These include preterm labor, placental abruption and premature rupture of the membranes.
- Medicine. Your health care professional may prescribe medicine taken by mouth called indomethacin (Indocin). It’s used for 48 hours to help decrease contractions and reduce amniotic fluid volume. Ask your care team to talk with you about the possible side effects.
After treatment, your health care team likely will want to check your amniotic fluid level about every 1 to 3 weeks.
If you have mild to moderate polyhydramnios, your care team probably will plan to have you deliver your baby at 39 or 40 weeks. If you have severe polyhydramnios, your team likely will talk about the right timing of delivery. The goal is to lower the chances of health problems for you and your baby.
Having polyhydramnios can be stressful. But your health care team is there for you. Work together to ensure that you and your baby receive the best possible care.
Preparing for an appointment
You’re likely to start by talking with your pregnancy care professional. Here’s some information to help you get ready for your appointment.
What you can do
Before your appointment:
- Write down any symptoms you’ve been having. Include when they started and how they’ve changed over time.
- Write down key personal information, including any other medical conditions for which you’re being treated.
- Make a list of all medicines, vitamins or supplements that you’re taking. Include the amounts you take, called the doses.
- Ask a friend or family member to join you. Having someone else with you at the checkup may help you remember something that you forgot or missed.
- Write down questions to ask your health care team.
Preparing a list of questions will help you make the most of your time with your doctor and other health care professionals. For polyhydramnios, some basic questions to ask include:
- What kind of tests do I need? How soon do I need to be tested?
- What treatment approach do you recommend?
- Do I need to limit any of my activities?
- What emergency symptoms should I watch for at home?
- How could this condition affect my baby?
- If I get pregnant again, will this happen again?
- Do you have any printed information that I can take with me? What websites do you recommend for more information?
What to expect from your doctor
Your health care professional likely will give you a physical exam and run some tests, including an ultrasound. You might be asked questions such as:
- When did you start having symptoms?
- Have your symptoms been constant or do they come and go?
- Do you have shortness of breath?
- Have you felt any lightheadedness or dizziness?
- Have you noticed an increase in swelling? Does it seem like you’re retaining more fluid than usual?
- What, if anything, seems to make your symptoms better?
- What, if anything, appears to make your symptoms worse?


