Aortic dissection
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
This life-threatening condition occurs when blood leaks through a tear in the body’s main artery (aorta). Know the symptoms and how it’s treated.
Overview
, Overview, ,
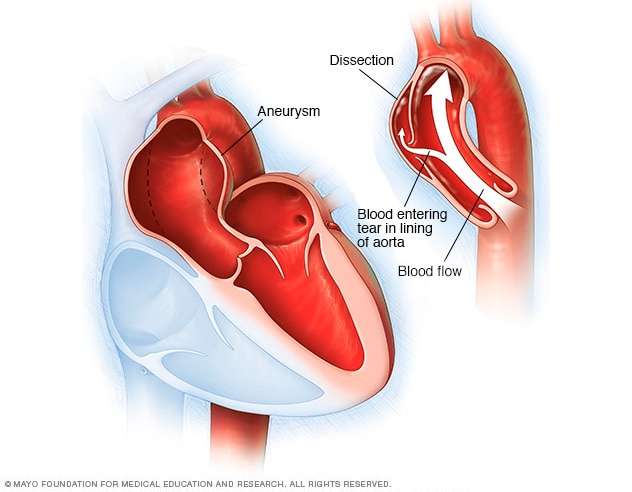
An aortic dissection is a serious condition in which a tear occurs in the inner layer of the body’s main artery (aorta). Blood rushes through the tear, causing the inner and middle layers of the aorta to split (dissect). If the blood goes through the outside aortic wall, aortic dissection is often deadly.
Aortic dissection is relatively uncommon. It usually occurs in men in their 60s and 70s. Symptoms of aortic dissection may mimic those of other diseases, often leading to delays in diagnosis. However, when an aortic dissection is detected early and treated promptly, the chance of survival greatly improves.
Aortic dissection symptoms may be similar to those of other heart problems, such as a heart attack. Typical signs and symptoms include:
- Sudden severe chest or upper back pain, often described as a tearing or ripping sensation, that spreads to the neck or down the back
- Sudden severe stomach pain
- Loss of consciousness
- Shortness of breath
- Symptoms similar to those of a stroke, including sudden vision problems, difficulty speaking, and weakness or loss of movement (paralysis) on one side of your body
- Weak pulse in one arm or thigh compared with the other
- Leg pain
- Difficulty walking
When to see a doctor
If you have severe chest pain, fainting, sudden shortness of breath or symptoms of a stroke, call 911 or your local emergency number. These signs and symptoms aren’t always due to a serious problem, but it’s best to be seen by a doctor quickly. Early detection and treatment may help save your life.
Causes
An aortic dissection is caused by a weakened area of the aorta’s wall.
Aortic dissections are divided into two groups, depending on which part of the aorta is affected:
- Type A. This more common and dangerous type involves a tear in the part of the aorta where it exits the heart. The tear may also occur in the upper aorta (ascending aorta), which may extend into the abdomen.
- Type B. This type involves a tear in the lower aorta only (descending aorta), which may also extend into the abdomen.
Risk factors
Some of the things that may raise your risk of aortic dissection include:
- Uncontrolled high blood pressure (hypertension)
- Hardening of the arteries (atherosclerosis)
- Weakened and bulging artery (aortic aneurysm)
- An aortic valve defect (bicuspid aortic valve)
- A narrowing of the aorta at birth (aortic coarctation)
Certain genetic diseases increase the risk of having an aortic dissection, including:
- Turner syndrome. High blood pressure, heart problems and other health conditions may result from this disorder.
- Marfan syndrome. This is a condition in which connective tissue, which supports various structures in the body, is weak. People with this disorder often have a family history of aneurysms of the aorta and other blood vessels or family history of aortic dissections.
- Other connective tissue disorders. This includes Ehlers-Danlos syndrome, a group of connective tissue disorders that involve loose joints and fragile blood vessels and Loeys-Dietz syndrome, which causes twisted arteries, especially in the neck.
Inflammation of the arteries (giant cell arteritis) may also increase your risk of aortic dissection.
Other potential risk factors for aortic dissection include:
- Sex. Men are more likely to have aortic dissection than women.
- Age. Aortic dissection is more likely in people age 60 and older.
- Cocaine use. This drug temporarily raises blood pressure.
- Pregnancy. Infrequently, aortic dissections occur in otherwise healthy women during pregnancy.
- High-intensity weightlifting. This and other strenuous resistance training may raise your risk of aortic dissection by increasing blood pressure during the activity.
Complications
Possible complications of aortic dissection include:
- Death due to severe internal bleeding
- Organ damage, such as kidney failure or life-threatening intestinal damage
- Stroke
- Aortic valve damage (aortic regurgitation) or rupture into the lining around the heart (cardiac tamponade)
Prevention
You can reduce your risk of an aortic dissection by preventing chest injury and taking steps to keep your heart healthy.
- Control blood pressure. If you have high blood pressure, get a home blood pressure measuring device to help you monitor your blood pressure.
- Don’t smoke. If you do smoke, take steps to stop.
- Maintain an ideal weight. Follow a low-salt diet with plenty of fruits, vegetables and whole grains and exercise regularly.
- Wear a seat belt. This reduces the risk of chest injury during a car accident.
-
Work with your doctor. If you have a family history of aortic dissection, a connective tissue disorder or a bicuspid aortic valve, tell your doctor. If you have an aortic aneurysm, find out how often you need monitoring and if surgery is necessary to repair your aneurysm.
If you have a genetic condition that increases your risk of aortic dissection, your doctor may recommend medications, even if your blood pressure is normal.
Diagnosis
Detecting an aortic dissection can be a challenge because the symptoms are similar to those of many other health problems. Your doctor may think you have an aortic dissection if you have:
- Sudden tearing or ripping chest pain
- Blood pressure difference between the right and left arms
- Widening of the aorta on chest X-ray
Tests to diagnose aortic dissection include:
- Transesophageal echocardiogram (TEE). This test uses sound waves to create pictures of the heart in motion. A is a special type of echocardiogram in which an ultrasound probe (transducer) is guided through your esophagus and placed close to your heart. This test gives your doctor a clearer picture of your heart and aorta than would a regular echocardiogram.
- Computerized tomography (CT) scan of the chest. X-ray are used to produce cross-sectional images of the body. A CT of the chest can confirm a diagnosis of aortic dissection.
- Magnetic resonance angiogram (MRA). An MRA uses a magnetic field and radio wave energy to create images of your blood vessels.
Treatment
An aortic dissection is a medical emergency requiring immediate treatment. Treatment may include surgery or medications, depending on the area of the aorta involved.
Type A aortic dissection
Treatment for type A aortic dissection may include:
- Surgery. Surgeons remove as much of the dissected aorta as possible and stop blood from leaking into the aortic wall. A synthetic tube (graft) is used to reconstruct the aorta. If the aortic valve leaks as a result of the damaged aorta, it may be replaced at the same time. The new valve is placed within the graft.
- Medications. Medications are given to reduce heart rate and lower blood pressure, which can prevent the aortic dissection from worsening. They may be given to people with type A aortic dissection to control blood pressure before surgery.
Type B aortic dissection
Treatment of type B aortic dissection may include:
- Medications. The same medications that are used to treat type A aortic dissection may be used without surgery to treat type B aortic dissections.
- Surgery. The procedure is similar to that used to correct a type A aortic dissection. Sometimes stents — small wire mesh tubes that act as a sort of scaffolding — may be placed in the aorta to repair complicated type B aortic dissections.
After treatment, you may need to take medication to control your blood pressure for the rest of your life. You may need regular CT scans or MRI scans to monitor your condition.


