Small intestinal bacterial overgrowth (SIBO)
![]() January, 3rd, 2025
January, 3rd, 2025
Benefit Summary
Small intestinal bacterial overgrowth (SIBO) can occur when excess bacteria builds up in the small intestine. Learn more about this bowel disorder.
Overview
, Overview, ,
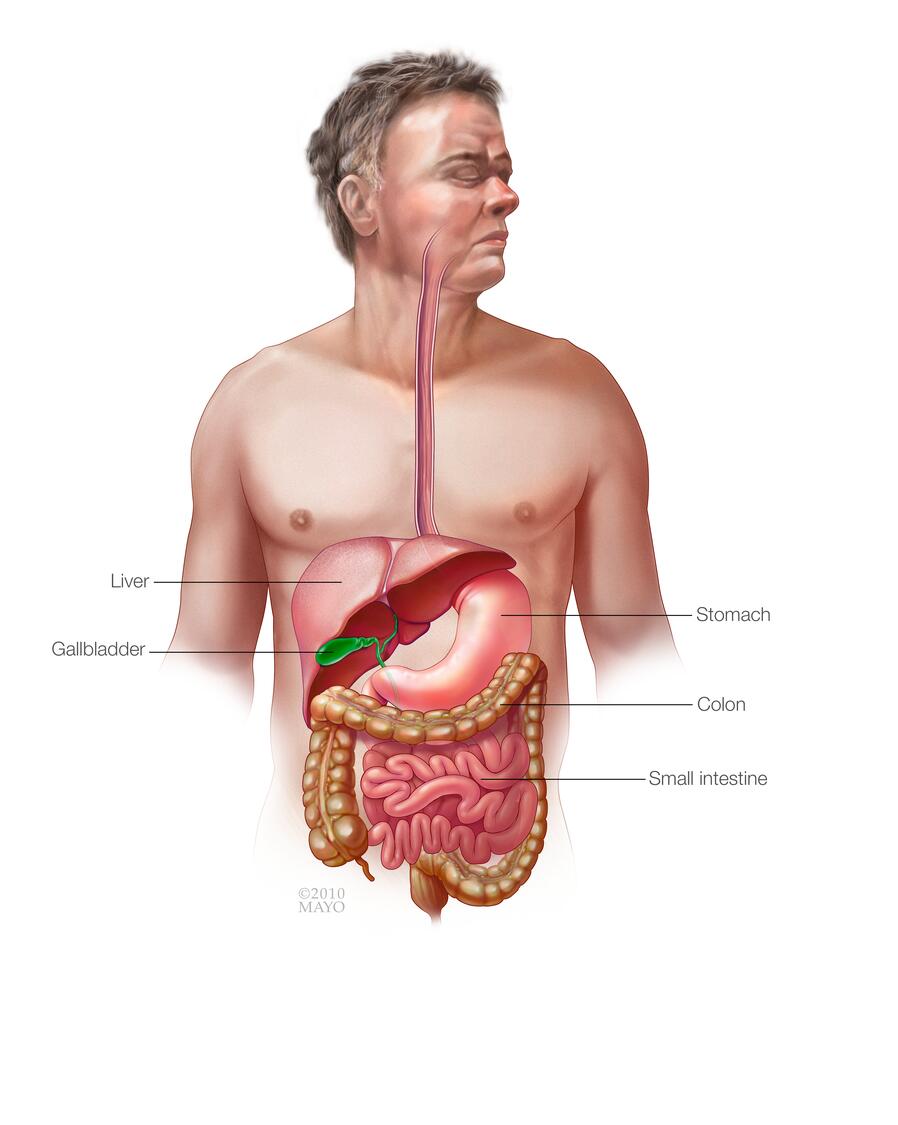
Small intestinal bacterial overgrowth (SIBO) occurs when there is an abnormal increase in the overall bacterial population in the small intestine — particularly types of bacteria not commonly found in that part of the digestive tract. This condition is sometimes called blind loop syndrome.
SIBO commonly results when a circumstance — such as surgery or disease — slows the passage of food and waste products in the digestive tract, creating a breeding ground for bacteria. The excess bacteria often cause diarrhea and may cause weight loss and malnutrition.
While SIBO is often a complication of stomach (abdominal) surgery, this condition can also result from structural problems and some diseases. Sometimes surgery is needed to correct the problem, but antibiotics are the most common treatment.
Symptoms
Signs and symptoms of small intestinal bacterial overgrowth (SIBO) often include:
- Loss of appetite
- Abdominal pain
- Nausea
- Bloating
- An uncomfortable feeling of fullness after eating
- Diarrhea
- Unintentional weight loss
- Malnutrition
When to see a doctor
Bloating, nausea and diarrhea are signs and symptoms of many intestinal problems. See your doctor for a full evaluation — especially if you’ve had abdominal surgery — if you have:
- Persistent diarrhea
- Rapid, unintentional weight loss
- Abdominal pain lasting more than a few days
If you have severe abdominal pain, seek immediate medical care.
Causes
Small intestinal bacterial overgrowth (SIBO) can be caused by:
- Complications of abdominal surgery, including gastric bypass for obesity and gastrectomy to treat peptic ulcers and stomach cancer
- Structural problems in and around your small intestine, including scar tissue (intestinal adhesions) that can wrap around the outside of the small bowel, and bulging pouches of tissue that protrude through the wall of the small intestine (intestinal diverticulosis)
- Certain medical conditions, including Crohn’s disease, radiation enteritis, scleroderma, celiac disease, diabetes or other conditions that can slow movement (motility) of food and waste products through the small intestine
Why small intestinal bacterial overgrowth (SIBO) develops
The small intestine is the longest section of your digestive tract, measuring about 20 feet (6.1 meters). The small intestine is where food mixes with digestive juices and nutrients are absorbed into your bloodstream.
Unlike your large intestine (colon), your small intestine normally has relatively few bacteria due to rapid flow of contents and the presence of bile. But in SIBO, stagnant food in the bypassed small intestine becomes an ideal breeding ground for bacteria. The bacteria may produce toxins as well as interfere with the absorption of nutrients. The breakdown products following bacterial digestion of food can also trigger diarrhea.
Factors that increase your risk of SIBO include:
- Gastric surgery for obesity or ulcers
- A structural defect in the small intestine
- An injury to the small intestine
- An abnormal passageway (fistula) between two segments of bowel
- Crohn’s disease, intestinal lymphoma or scleroderma involving the small intestine
- History of radiation therapy to the abdomen
- Diabetes
- Diverticulosis of the small intestine
- Adhesions caused by previous abdominal surgery
Complications
Small intestinal bacterial overgrowth (SIBO) can cause escalating problems, including:
-
Poor absorption of fats, carbohydrates and proteins. Bile salts, which are normally needed to digest fats, are broken down by the excess bacteria in your small intestine, resulting in incomplete digestion of fats and diarrhea. Bacterial products may also harm the mucous lining (mucosa) of the small intestine, resulting in decreased absorption of carbohydrates and proteins.
Bacteria can compete for available food. And compounds produced through the bacterial break-down of stagnant food can also trigger diarrhea. Together, these effects of bacterial overgrowth result in diarrhea, malnutrition and weight loss.
-
Vitamin deficiency. As a result of incomplete absorption of fats, your body can’t fully absorb the fat-soluble vitamins A, D, E and K. Bacteria in the small intestine synthesize as well as use vitamin B-12, which is essential for the normal functioning of your nervous system and the production of blood cells and DNA.
The overgrowth of bacteria can result in B-12 deficiency that can lead to weakness, fatigue, tingling, and numbness in your hands and feet and, in advanced cases, to mental confusion. Damage to your central nervous system resulting from B-12 deficiency may be irreversible.
- Weakened bones (osteoporosis). Over time, damage to your intestine from abnormal bacterial growth causes poor calcium absorption, and eventually may lead to bone diseases, such as osteoporosis.
- Kidney stones. Poor calcium absorption may also eventually result in kidney stones.
Diagnosis
In order to diagnose small intestinal bacterial overgrowth (SIBO), you may have tests to check for bacterial overgrowth in your small intestine, poor fat absorption, or other problems that may be causing or contributing to your symptoms. Common tests include:
- Breath testing. This type of noninvasive test measures the amount of hydrogen or methane that you breathe out after drinking a mixture of glucose and water. A rapid rise in exhaled hydrogen or methane may indicate bacterial overgrowth in your small intestine. Although widely available, breath testing is less specific than other types of tests for diagnosing bacterial overgrowth.
- Small intestine aspirate and fluid culture. Removing and testing fluid from the small intestine used to be considered a good way to diagnose SIBO. However, this technique can lead to a diagnosis of SIBO that is not correct due to contamination from bacteria in the mouth. Experts no longer recommend this test.
In addition to these tests, your doctor may recommend blood testing to look for vitamin deficiency or a stool evaluation to test for fat malabsorption. In some cases, your doctor may recommend imaging tests, such as X-rays, computerized tomography (CT) scanning or magnetic resonance imaging (MRI) to look for structural abnormalities of the intestine.
Treatment
Whenever possible, doctors treat small intestinal bacterial overgrowth (SIBO) by dealing with the underlying problem — for example, by surgically repairing a postoperative loop, stricture or fistula. But a loop can’t always be reversed. In that case, treatment focuses on correcting nutritional deficiencies and eliminating bacterial overgrowth.
Antibiotic therapy
For most people, the initial way to treat bacterial overgrowth is with antibiotics. Doctors may start this treatment if your symptoms and medical history strongly suggest this is the cause, even when test results are inconclusive or without any testing at all. Testing may be performed if antibiotic treatment is not effective.
A short course of antibiotics often significantly reduces the number of abnormal bacteria. But bacteria can return when the antibiotic is discontinued, so treatment may need to be long term. Some people with a loop in their small intestine may go for long periods without needing antibiotics, while others may need them regularly.
Doctors may also switch among different antibiotics to help prevent bacterial resistance. Antibiotics wipe out most intestinal bacteria, both normal and abnormal. As a result, antibiotics can cause some of the very problems they’re trying to cure, including diarrhea. Switching among different drugs can help avoid this problem.
Nutritional support
Correcting nutritional deficiencies is a crucial part of treating SIBO, particularly in people with severe weight loss. Malnutrition can be treated, but the damage it causes can’t always be reversed.
These treatments may improve vitamin deficiencies, reduce intestinal distress and help with weight gain:
- Nutritional supplements. People with SIBO may need intramuscular injections of vitamin B-12, as well as oral vitamins, calcium and iron supplements.
-
Lactose-free diet. Damage to the small intestine may cause you to lose the ability to digest milk sugar (lactose). In that case, it’s important to avoid most lactose-containing products, or use lactase preparations that help digest milk sugar.
Some affected people may tolerate yogurt because the bacteria used in the culturing process naturally break down lactose.
Preparing for your appointment
If you have signs and symptoms that are common to small intestinal bacterial overgrowth (SIBO), make an appointment with your doctor. After an initial evaluation, you may be referred to a doctor who specializes in treatment of digestive disorders (gastroenterologist).
Here’s some information to help you get ready for your appointment, and what to expect from your doctor.
- Write down your symptoms, including when they started and how they may have changed or worsened over time.
- Bring your medical records, especially if you have had surgery on your stomach or intestines, have any known bowel condition, or have received radiation to the abdomen or pelvis.
- Make a list of all your medications, vitamins and supplements.
- Write down your key medical information, including other conditions with which you’ve been diagnosed. Be sure to let your doctor know about any abdominal surgery you’ve had.
- Write down key personal information, including any recent changes or stressors in your life. These factors can be connected to digestive signs and symptoms.
- Take a family member or friend along, if possible. It can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor. Creating your list of questions in advance can help you make the most of your time with your doctor.
Don’t hesitate to ask questions. Some basic questions to ask your doctor include:
- What is the most likely cause of my condition?
- What treatment approach do you recommend?
- Are there any side effects associated with the medications you’re prescribing?
- I have other conditions. How can I treat them?
- Will I need to stay on medications long term?
- How often will you see me to monitor my progress?
- Should I take any nutritional supplements?
- Do I have any vitamin deficiencies?
- Are there any lifestyle or dietary changes I can make to help reduce or manage my symptoms?
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may reserve time to go over points you want to spend more time on. You may be asked:
- Have you ever had abdominal surgery?
- What are your symptoms?
- When did you first notice these symptoms?
- Do your symptoms come and go or stay about the same?
- Is your pain cramp-like?
- Does your pain radiate to other parts of your abdomen or to your back?
- Have you lost weight without trying?
- Have you noticed a change in your stools?
- Have your signs and symptoms included vomiting?
- Have your signs and symptoms included a fever?
- Has anyone close to you had similar signs or symptoms recently?
- What is your typical daily diet?
- Have you ever been diagnosed with a food allergy or with lactose intolerance?
- Have you been diagnosed with any other medical conditions?
- What medications are you taking, including prescription and over-the-counter medications, vitamins, herbs, and supplements?
- Do you have any family history of bowel disorders or colon cancer?
- Have you ever had radiation therapy to your abdomen or pelvis?
- Have you ever had kidney stones?
- Have you ever had problems with your pancreas?
- Do you have Crohn’s disease?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



