Heart attack
![]() October, 9th, 2023
October, 9th, 2023
Benefit Summary
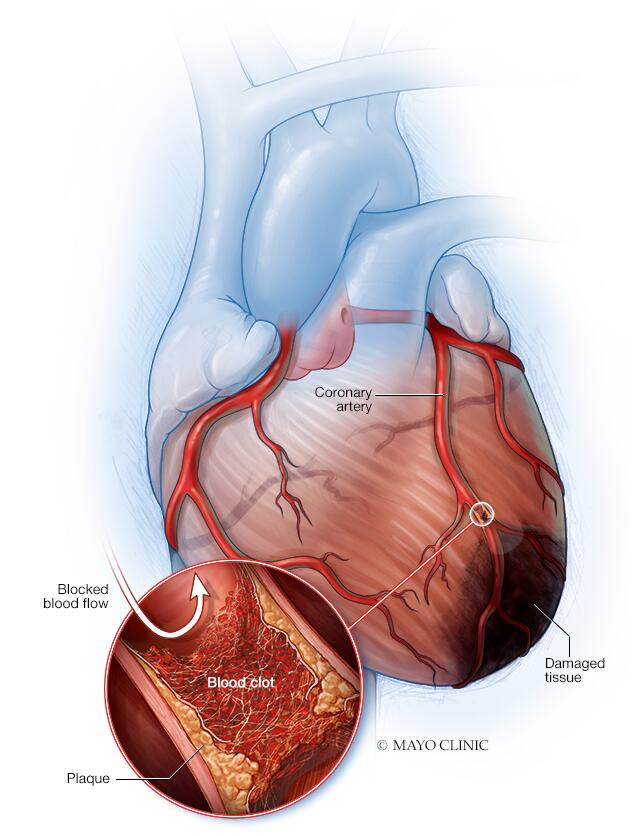
A blockage of blood flow to the heart can damage or destroy heart muscle.
Overview
, Overview, ,
A heart attack occurs when the flow of blood to the heart is severely reduced or blocked. The blockage is usually due to a buildup of fat, cholesterol and other substances in the heart (coronary) arteries. The fatty, cholesterol-containing deposits are called plaques. The process of plaque buildup is called atherosclerosis.
Sometimes, a plaque can rupture and form a clot that blocks blood flow. A lack of blood flow can damage or destroy part of the heart muscle.
A heart attack is also called a myocardial infarction.
Prompt treatment is needed for a heart attack to prevent death. Call 911 or emergency medical help if you think you might be having a heart attack.
Symptoms of a heart attack vary. Some people have mild symptoms. Others have severe symptoms. Some people have no symptoms.
Common heart attack symptoms include:
- Chest pain that may feel like pressure, tightness, pain, squeezing or aching
- Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly
- Cold sweat
- Fatigue
- Heartburn or indigestion
- Lightheadedness or sudden dizziness
- Nausea
- Shortness of breath
Women may have atypical symptoms such as brief or sharp pain felt in the neck, arm or back. Sometimes, the first symptom sign of a heart attack is sudden cardiac arrest.
Some heart attacks strike suddenly. But many people have warning signs and symptoms hours, days or weeks in advance. Chest pain or pressure (angina) that keeps happening and doesn’t go away with rest may be an early warning sign. Angina is caused by a temporary decrease in blood flow to the heart.
When to see a doctor
Get help right away if you think you’re having a heart attack. Take these steps:
- Call for emergency medical help. If you think you’re having a heart attack, immediately call 911 or your local emergency number. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only if there are no other options.
- Take nitroglycerin, if prescribed to you by a health care provider. Take it as instructed while awaiting emergency help.
-
Take aspirin, if recommended. Taking aspirin during a heart attack may reduce heart damage by preventing blood clotting.
Aspirin can interact with other drugs. Don’t take an aspirin unless your care provider or emergency medical personnel say to do so. Don’t delay calling 911 to take an aspirin. Call for emergency help first.
What to do if you see someone who might be having a heart attack
If someone is unconscious and you think they’re having a heart attack, first call 911 or your local emergency number. Then check if the person is breathing and has a pulse. If the person isn’t breathing or you don’t find a pulse, only then should you begin CPR.
- If you’re untrained in CPR, do hands-only CPR. That means push hard and fast on the person’s chest — about 100 to 120 compressions a minute.
- If you’re trained in CPR and confident in your ability, start with 30 chest compressions before giving two rescue breaths.
Causes
Coronary artery disease causes most heart attacks. In coronary artery disease, one or more of the heart (coronary) arteries are blocked. This is usually due to cholesterol-containing deposits called plaques. Plaques can narrow the arteries, reducing blood flow to the heart.
If a plaque breaks open, it can cause a blood clot in the heart.
A heart attack may be caused by a complete or partial blockage of a heart (coronary) artery. One way to classify heart attacks is whether an electrocardiogram (ECG or EKG) shows some specific changes (ST elevation) that require emergency invasive treatment. Your health care provider may use ECG results to describe these types of heart attacks.
- An acute complete blockage of a medium or large heart artery usually means you’ve had an ST elevation myocardial infarction (STEMI).
- A partial blockage often means you’ve had a non-ST elevation myocardial infarction (NSTEMI). However, some people with NSTEMI have a total blockage.
Not all heart attacks are caused by blocked arteries. Other causes include:
- Coronary artery spasm. This is a severe squeezing of a blood vessel that’s not blocked. The artery generally has cholesterol plaques or there is early hardening of the vessel due to smoking or other risk factors. Other names for coronary artery spasms are Prinzmetal’s angina, vasospastic angina or variant angina.
- Certain infections. COVID-19 and other viral infections may cause damage to the heart muscle.
- Spontaneous coronary artery dissection (SCAD). This life-threatening condition is caused by a tear inside a heart artery.
Risk factors
Heart attack risk factors include:
- Age. Men age 45 and older and women age 55 and older are more likely to have a heart attack than are younger men and women.
- Tobacco use. This includes smoking and long-term exposure to secondhand smoke. If you smoke, quit.
- High blood pressure. Over time, high blood pressure can damage arteries that lead to the heart. High blood pressure that occurs with other conditions, such as obesity, high cholesterol or diabetes, increases the risk even more.
- High cholesterol or triglycerides. A high level of low-density lipoprotein (LDL) cholesterol (the “bad” cholesterol) is most likely to narrow arteries. A high level of certain blood fats called triglycerides also increases heart attack risk. Your heart attack risk may drop if levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — are in the standard range.
- Obesity. Obesity is linked with high blood pressure, diabetes, high levels of triglycerides and bad cholesterol, and low levels of good cholesterol.
- Diabetes. Blood sugar rises when the body doesn’t make a hormone called insulin or can’t use it correctly. High blood sugar increases the risk of a heart attack.
- Metabolic syndrome. This is a combination of at least three of the following things: enlarged waist (central obesity), high blood pressure, low good cholesterol, high triglycerides and high blood sugar. Having metabolic syndrome makes you twice as likely to develop heart disease than if you don’t have it.
- Family history of heart attacks. If a brother, sister, parent or grandparent had an early heart attack (by age 55 for males and by age 65 for females), you might be at increased risk.
- Not enough exercise. A lack of physical activity (sedentary lifestyle) is linked to a higher risk of heart attacks. Regular exercise improves heart health.
- Unhealthy diet. A diet high in sugars, animal fats, processed foods, trans fats and salt increases the risk of heart attacks. Eat plenty of fruits, vegetables, fiber and healthy oils.
- Stress. Emotional stress, such as extreme anger, may increase the risk of a heart attack.
- Illegal drug use. Cocaine and amphetamines are stimulants. They can trigger a coronary artery spasm that can cause a heart attack.
- A history of preeclampsia. This condition causes high blood pressure during pregnancy. It increases the lifetime risk of heart disease.
- An autoimmune condition. Having a condition such as rheumatoid arthritis or lupus can increase the risk of a heart attack.
Complications
Heart attack complications are often due to heart muscle damage. Potential complications of a heart attack include:
- Irregular or atypical heart rhythms (arrhythmias). Heart attack damage can affect how electrical signals move through the heart, causing heartbeat changes. Some may be serious and can be deadly.
- Cardiogenic shock. This rare condition occurs when the heart is suddenly and abruptly unable to pump blood.
- Heart failure. A lot of damage to the heart muscle tissue can make the heart unable to pump blood. Heart failure can be temporary or long-lasting (chronic).
- Inflammation of the saclike tissue surrounding the heart (pericarditis). Sometimes a heart attack triggers a faulty immune system response. This condition may be called Dressler syndrome, postmyocardial infarction syndrome or postcardiac injury syndrome.
- Cardiac arrest. Without warning, the heart stops. A sudden change in the heart’s signaling causes sudden cardiac arrest. A heart attack increases the risk of this life-threatening condition. It can lead to death (sudden cardiac death) without immediate treatment.
Prevention
It’s never too late to take steps to prevent a heart attack — even if you’ve already had one. Here are ways to prevent a heart attack.
- Follow a healthy lifestyle. Don’t smoke. Maintain a healthy weight with a heart-healthy diet. Get regular exercise and manage stress.
- Manage other health conditions. Certain conditions, such as high blood pressure and diabetes, can increase the risk of heart attacks. Ask your health care provider how often you need checkups.
- Take medications as directed. Your health care provider may prescribe drugs to protect and improve your heart health.
It’s also a good idea to learn CPR properly so you can help someone who’s having a heart attack. Consider taking an accredited first-aid training course, including CPR and how to use an automated external defibrillator (AED).
Diagnosis
Ideally, a health care provider should screen you during regular checkups for risk factors that can lead to a heart attack.
A heart attack is often diagnosed in an emergency setting. If you’ve had or are having a heart attack, care providers will take immediate steps to treat your condition. If you’re able to answer questions, you may be asked about your symptoms and medical history.
Diagnosis of a heart attack includes checking blood pressure, pulse and temperature. Tests are done to see how the heart is beating and to check overall heart health.
Tests
Tests to diagnose a heart attack include:
- Electrocardiogram (ECG or EKG). This first test done to diagnose a heart attack records electrical signals as they travel through the heart. Sticky patches (electrodes) are attached to the chest and sometimes the arms and legs. Signals are recorded as waves displayed on a monitor or printed on paper. An ECG can show if you are having or have had a heart attack.
- Blood tests. Certain heart proteins slowly leak into the blood after heart damage from a heart attack. Blood tests can be done to check for these proteins (cardiac markers).
- Chest X-ray. A chest X-ray shows the condition and size of the heart and lungs.
- Echocardiogram. Sound waves (ultrasound) create images of the moving heart. This test can show how blood moves through the heart and heart valves. An echocardiogram can help identify whether an area of your heart has been damaged.
- Coronary catheterization (angiogram). A long, thin tube (catheter) is inserted into an artery, usually in the leg, and guided to the heart. Dye flows through the catheter to help the arteries show up more clearly on images made during the test.
- Cardiac CT or MRI. These tests create images of the heart and chest. Cardiac CT scans use X-rays. Cardiac MRI uses a magnetic field and radio waves to create images of your heart. For both tests, you usually lie on a table that slides inside a long tubelike machine. Each test can be used to diagnose heart problems. They can help show the severity of heart damage.
Treatment
Each minute after a heart attack, more heart tissue is damaged or dies. Urgent treatment is needed to fix blood flow and restore oxygen levels. Oxygen is given immediately. Specific heart attack treatment depends on whether there’s a partial or complete blockage of blood flow.
Medications
Medications to treat a heart attack might include:
- Aspirin. Aspirin reduces blood clotting. It helps keep blood moving through a narrowed artery. If you called 911 or your local emergency number, you may be told to chew aspirin. Emergency medical providers may give you aspirin immediately.
- Clot busters (thrombolytics or fibrinolytics). These drugs help break up any blood clots that are blocking blood flow to the heart. The earlier a thrombolytic drug is given after a heart attack, the less the heart is damaged and the greater the chance of survival.
- Other blood-thinning medicines. A medicine called heparin may be given by an IV injection. Heparin makes the blood less sticky and less likely to form clots.
- Nitroglycerin. This medication widens the blood vessels. It helps improve blood flow to the heart. Nitroglycerin is used to treat sudden chest pain (angina). It’s given as a pill under the tongue, as a pill to swallow or as an injection.
- Morphine. This medicine is given to relieve chest pain that doesn’t go away with nitroglycerin.
- Beta blockers. These medications slow the heartbeat and decrease blood pressure. Beta blockers can limit the amount of heart muscle damage and prevent future heart attacks. They are given to most people who are having a heart attack.
- Blood pressure medicines called ACE inhibitors. These drugs lower blood pressure and reduce stress on the heart.
- Statins. These drugs help lower unhealthy cholesterol levels. Too much bad (low-density lipoprotein, or LDL) cholesterol can clog arteries.
Surgical and other procedures
If you’ve had a heart attack, a surgery or procedure may be done to open a blocked artery. Surgeries and procedures to treat a heart attack include:
-
Coronary angioplasty and stenting. This procedure is done to open clogged heart arteries. It may also be called percutaneous coronary intervention (PCI). If you’ve had a heart attack, this procedure is often done during a procedure to find blockages (cardiac catheterization).
During angioplasty, a heart doctor (cardiologist) guides a thin, flexible tube (catheter) to the narrowed part of the heart artery. A tiny balloon is inflated to help widen the blocked artery and improve blood flow.
A small wire mesh tube (stent) may be placed in the artery during angioplasty. The stent helps keep the artery open. It lowers the risk of the artery narrowing again. Some stents are coated with a medication that helps keep the arteries open.
- Coronary artery bypass grafting (CABG). This is open-heart surgery. A surgeon takes a healthy blood vessel from another part of the body to create a new path for blood in the heart. The blood then goes around the blocked or narrowed coronary artery. It may be done as an emergency surgery at the time of a heart attack. Sometimes it’s done a few days later, after the heart has recovered a bit.
Cardiac rehabilitation
Cardiac rehabilitation is a personalized exercise and education program that teaches ways to improve heart health after heart surgery. It focuses on exercise, a heart-healthy diet, stress management and a gradual return to usual activities. Most hospitals offer cardiac rehabilitation starting in the hospital. The program typically continues for a few weeks or months after you return home.
People who attend cardiac rehab after a heart attack generally live longer and are less likely to have another heart attack or complications from the heart attack. If cardiac rehab is not recommended during your hospital stay, ask your provider about it.
Self care
To improve heart health, take the following steps:
- Exercise. Regular exercise helps improve heart health. As a general goal, aim for at least 30 minutes of moderate or vigorous physical activity five or more days a week. If you’ve had a heart attack or heart surgery, you may have activity restrictions. Ask your health care provider what’s best for you.
- Eat a heart-healthy diet. Avoid or limit foods with a lot of saturated fat, trans fats, salt and sugar. Choose whole grains, fruits, vegetables, and lean proteins, such as fish and beans.
- Maintain a healthy weight. Too much weight strains the heart. Being overweight increases the risk of high cholesterol, high blood pressure and diabetes.
- Don’t smoke. Quitting smoking is the most important thing you can do to improve heart health. Also, avoid being around secondhand smoke. If you need to quit, ask your provider for help.
- Limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Get regular health checkups. Some of the major risk factors for a heart attack — high blood cholesterol, high blood pressure and diabetes — don’t cause early symptoms.
- Manage blood pressure, cholesterol and blood sugar. Ask your provider how often you need to have your blood pressure, blood sugar and cholesterol levels checked.
- Control stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to ease stress.
Coping and support
Having a heart attack is scary. Talking about your feelings with your care provider, a family member or a friend might help. Or consider talking to a mental health care provider or joining a support group. Support groups let you connect with others who have been through similar events.
If you feel sad, scared or depressed, tell your care provider. Cardiac rehabilitation programs can help prevent or treat depression after a heart attack.
Sex after a heart attack
Some people worry about having sex after a heart attack. Most people can safely return to sexual activity after recovery. But talk to your care provider first. When you can resume sex may depend on your physical comfort, emotional readiness and previous sexual activity.
Some heart medications can affect sexual function. If you’re having problems with sexual dysfunction, talk to your care provider.
Preparing for your appointment
A heart attack usually is diagnosed in an emergency setting. However, if you’re concerned about your risk of a heart attack, talk to your care provider. A cardiovascular risk assessment can be done to determine your level of risk.
You may be referred to a doctor trained in heart diseases (cardiologist).
Here’s some information to help you prepare for your appointment.
What you can do
When you make the appointment, ask if there’s anything you need to do in advance, such as restrict your diet. You might need to avoid food or drink for a while before a cholesterol test, for example.
Make a list of:
- Your symptoms, including any that seem unrelated to heart disease, and when they began
- Family history of heart problems, including heart disease, stroke, high blood pressure, diabetes or early heart attacks
- Important personal information, including recent major stresses or recent life changes
- All medications, vitamins and other supplements you take, including doses
- Questions to ask your provider
Take a friend or relative along, if possible, to help you remember the information you’re given.
Some questions to ask your provider about heart attack prevention include:
- What tests do I need to determine my current heart health?
- What foods should I eat or avoid?
- What’s an appropriate level of physical activity?
- How often should I be screened for heart disease?
- I have other health conditions. How can I best manage these conditions together?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don’t hesitate to ask other questions.
What to expect from your doctor
Your health care provider is likely to ask you questions, including:
- How severe are your symptoms?
- Are they constant or do they come and go?
- What, if anything, seems to improve your symptoms?
- If you have chest pain, does it improve with rest?
- What, if anything, worsens your symptoms?
- If you have chest pain, does strenuous activity make it worse?
- Have you been diagnosed with high blood pressure, diabetes or high cholesterol?
What you can do in the meantime
It’s never too early to make healthy lifestyle changes, such as quitting smoking, eating healthy foods and becoming more active. These are important steps in preventing heart attacks and improving overall health.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



