Hip fracture
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
The risk of breaking a hip increases with age. Learn about lifestyle changes that can keep bones strong and reduce risk of breaking.
Overview
, Overview, ,
A hip fracture is a serious injury, with complications that can be life-threatening. The risk of hip fracture rises with age.
Risk increases because bones tend to weaken with age (osteoporosis). Multiple medications, poor vision and balance problems also make older people more likely to fall — one of the most common causes of hip fracture.
A hip fracture almost always requires surgical repair or replacement, followed by physical therapy. Taking steps to maintain bone density and avoid falls can help prevent a hip fracture.
Symptoms
Signs and symptoms of a hip fracture include:
- Inability to get up from a fall or to walk
- Severe pain in the hip or groin
- Inability to put weight on the leg on the side of the injured hip
- Bruising and swelling in and around the hip area
- Shorter leg on the side of the injured hip
- Outward turning of the leg on the side of the injured hip
Causes
A severe impact, such as a car crash, can cause hip fractures in people of all ages. In older adults, a hip fracture is most often a result of a fall from a standing height. In people with very weak bones, a hip fracture can occur simply by standing on the leg and twisting.
Risk factors
Many things can increase the risk of hip fractures.
Your age and sex
Bone density and muscle mass tend to decrease with age. Older people can also have problems with vision and balance, which can increase the risk of falling.
Hip fractures occur in women about three times more often than they do in men. Women lose bone density faster than men do, in part because the drop in estrogen levels that occurs with menopause accelerates bone loss. However, men also can develop dangerously low levels of bone density.
Medical conditions
The risk of hip fracture can be increased if you have:
- Osteoporosis. This condition weakens bones and makes them more likely to break.
- Thyroid problems. An overactive thyroid can lead to fragile bones.
- Intestinal disorders. Conditions that reduce absorption of vitamin D and calcium also can cause weakened bones.
- Problems with balance. Parkinson’s disease, stroke and peripheral neuropathy can increase the risk of falling. Having low blood sugar or low blood pressure also can contribute to the risk of falls.
Certain medications
Cortisone medications, such as prednisone, can weaken bones if taken long-term. Certain drugs or certain combinations of medications can cause dizziness, which can increase the risk of falling. The most common drugs associated with falls include sleep medications, antipsychotics and sedatives.
Nutritional problems
Lack of calcium and vitamin D in the diet of young people lowers peak bone mass and increases risk of fracture later in life. It’s also important to get enough calcium and vitamin D in older age to try to maintain bone density. Being underweight also increases the risk of bone loss.
Lifestyle choices
Lack of regular weight-bearing exercise, such as walking, can result in weakened bones and muscles, making falls and fractures more likely.
Tobacco and alcohol both can interfere with the normal processes of bone building and maintenance, resulting in bone loss.
Complications
A hip fracture can reduce independence and sometimes shorten life. About half the people who have a hip fracture aren’t able to regain the ability to live independently.
When hip fractures prevent movement for a long time, complications can include:
- Blood clots in the legs or lungs
- Bedsores
- Pneumonia
- Further loss of muscle mass, increasing the risk of falls and injuries
- Death
Prevention
Healthy lifestyle choices in early adulthood build a higher peak bone mass and reduce the risk of osteoporosis in later years. The same measures adopted at any age might lower the risk of falls and improve overall health.
To avoid falls and to maintain healthy bone:
- Get enough calcium and vitamin D. In general, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Exercise to strengthen bones and improve balance. Weight-bearing exercises, such as walking, help maintain peak bone density. Exercise also increases overall strength, decreasing the risk of falling. Balance training also is important to reduce the risk of falls since balance tends to deteriorate with age.
- Avoid smoking or excessive drinking. Tobacco and alcohol use can reduce bone density. Drinking too much alcohol can also impair balance and increase the risk of falling.
- Assess the home for hazards. Remove throw rugs, keep electrical cords against the wall, and clear excess furniture and anything else that could trip people. Make sure all rooms and passageways are well lit.
- Check your eyes. Have an eye exam every other year, or more often if you have diabetes or an eye disease.
- Use a cane, walking stick or walker. If you don’t feel steady when you walk, ask a health care provider or occupational therapist whether these aids might help.
Diagnosis
A health care provider can often diagnose a hip fracture based on symptoms and the abnormal position of the hip and leg. An X-ray usually will confirm the fracture and show where the fracture is.
If your X-ray doesn’t show a fracture but you still have hip pain, your provider might order an MRI or bone scan to look for a hairline fracture.
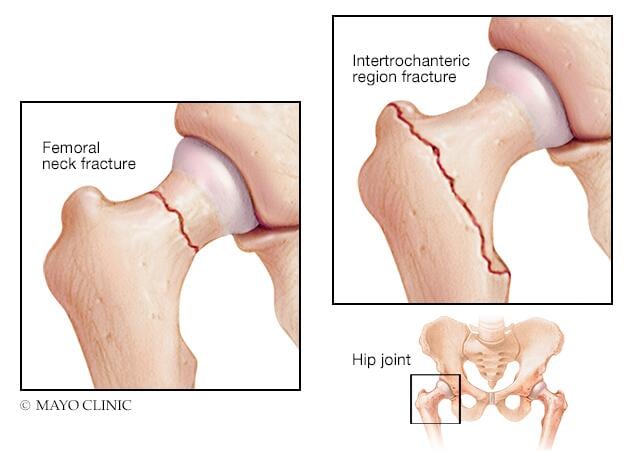
Most hip fractures occur in one of two locations on the long bone that extends from the pelvis to your knee (femur):
- The femoral neck. This area is situated in the upper portion of your femur, just below the ball part (femoral head) of the ball-and-socket joint.
- The intertrochanteric region. This region is a little farther down from the hip joint, in the portion of the upper femur that juts outward.
Treatment for hip fracture usually involves a combination of prompt surgical repair, rehabilitation, and medication to manage pain and to prevent blood clots and infection.
Surgery
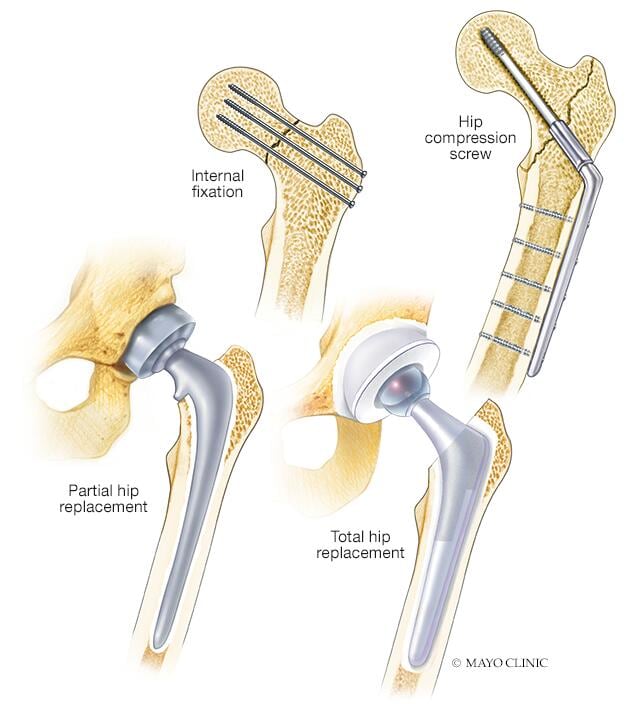
The type of surgery generally depends on where and how severe the fracture is, whether the broken bones aren’t properly aligned (displaced), and your age and underlying health conditions. Options include:
- Internal repair using screws. Metal screws are inserted into the bone to hold it together while the fracture heals. Sometimes screws are attached to a metal plate that runs down the thighbone (femur).
- Total hip replacement. The upper femur and the socket in the pelvic bone are replaced with artificial parts (prostheses). Increasingly, studies show total hip replacement to be more cost-effective and associated with better long-term outcomes in otherwise healthy adults who live independently.
- Partial hip replacement. In some situations, the socket part of the hip doesn’t need to be replaced. Partial hip replacement might be recommended for adults who have other health conditions or who no longer live independently.
Surgeons may recommend a full or partial hip replacement if the blood supply to the ball part of the hip joint was damaged during the fracture. That type of injury, which occurs most often in older people with femoral neck fractures, means the bone is less likely to heal properly.
Rehabilitation
Physical therapy will initially focus on range-of-motion and strengthening exercises. Depending on the type of surgery and whether there’s help at home, going to an extended care facility might be necessary.
In extended care and at home, an occupational therapist teaches techniques for independence in daily life, such as using the toilet, bathing, dressing and cooking. An occupational therapist will determine if a walker or wheelchair might be needed to regain mobility and independence.
You may be referred to an orthopedic surgeon.
What to expect
Your health care provider might ask:
- Have you recently fallen or had another injury to your hip?
- How severe is your pain?
- Can you put weight on your leg on the side of your injured hip?
- Have you had a bone density test?
- Have you been diagnosed with any other medical conditions? What medications do you take, including vitamins and supplements?
- Do you use alcohol or tobacco?
- Have you ever had surgery? Were there problems?
- Do any of your blood relatives — such as a parent or sibling — have a history of bone fractures or osteoporosis?
- Do you live independently?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



