Invasive lobular carcinoma
![]() November, 20th, 2024
November, 20th, 2024
Benefit Summary
Breast cancer that begins in the milk-producing glands of the breast is uncommon. Learn what sets lobular carcinoma apart from other breast cancer types.
Overview
, Overview, ,
Invasive lobular carcinoma is a type of breast cancer that begins as a growth of cells in the milk-producing glands of the breast. These glands are called lobules.
Invasive cancer means that the cancer cells have broken out of the lobule where they began and spread into the breast tissue. The cells have the potential to spread to the lymph nodes and other areas of the body.
Invasive lobular carcinoma makes up a small portion of all breast cancers. The most common type of breast cancer begins in the breast ducts. This type is called invasive ductal carcinoma.
Symptoms
At first, invasive lobular carcinoma may cause no signs and symptoms. As it grows larger, invasive lobular carcinoma may cause:
- A change in the texture or appearance of the skin over the breast, such as dimpling or thickening.
- A new area of fullness or swelling in the breast.
- A newly inverted nipple.
- An area of thickening in part of the breast.
Invasive lobular carcinoma is less likely to cause a firm or distinct breast lump than other types of breast cancer.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you notice a change in your breasts. Changes to look for may include a lump, an area of puckered or otherwise unusual skin, a thickened region under the skin, and nipple discharge.
Ask your healthcare professional when you should consider breast cancer screening and how often it should be repeated. Most healthcare professionals recommend considering routine breast cancer screening beginning in your 40s.
Causes
It’s not clear what causes invasive lobular carcinoma.
This form of breast cancer begins when cells in one or more milk-producing glands of the breast develop changes in their DNA. A cell’s DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
Invasive lobular carcinoma cells tend to invade breast tissue by spreading out rather than forming a firm lump. The affected area may have a different feel from the surrounding breast tissue. The area may feel more like a thickening and fullness, but it’s unlikely to feel like a lump.
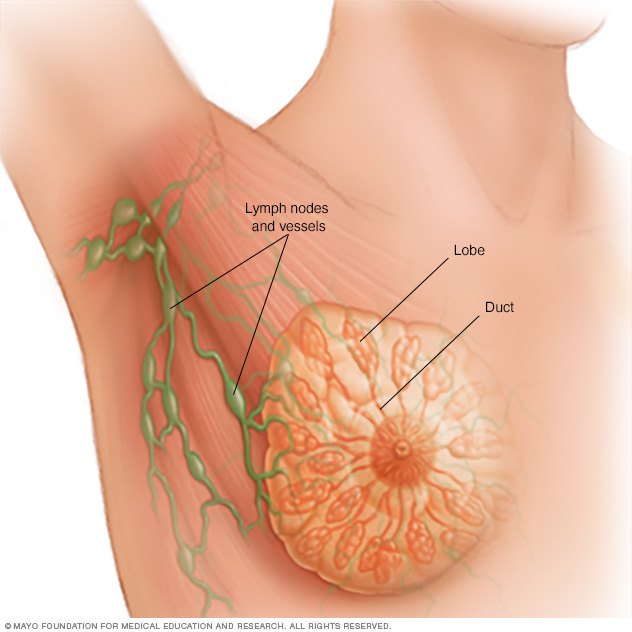
Each breast contains 15 to 20 lobes of glandular tissue, arranged like the petals of a daisy. The lobes are further divided into smaller lobules that produce milk for breastfeeding. Small tubes, called ducts, conduct the milk to a reservoir that lies just beneath the nipple.
Breast anatomy Risk factors
Risk factors for invasive lobular carcinoma are thought to be similar to the risk factors for breast cancer in general. Factors that may increase the risk of breast cancer include:
- A family history of breast cancer. If a parent, sibling or child had breast cancer, your risk of breast cancer is increased. The risk is higher if your family has a history of getting breast cancer at a young age. The risk also is higher if you have multiple family members with breast cancer. Still, most people diagnosed with breast cancer don’t have a family history of the disease.
- A personal history of breast cancer. If you’ve had cancer in one breast, you have an increased risk of getting cancer in the other breast.
- A personal history of breast conditions. Certain breast conditions are signs that you have a higher risk of breast cancer. These conditions include lobular carcinoma in situ, also called LCIS, and atypical hyperplasia of the breast. If you’ve had a breast biopsy that found one of these conditions, you have an increased risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. Beginning menopause after age 55 increases the risk of breast cancer.
- Being female. Women are much more likely than men are to get breast cancer. Everyone is born with some breast tissue, so anyone can get breast cancer.
- Dense breast tissue. Breast tissue is made up of fatty tissue and dense tissue. Dense tissue is made of milk glands, milk ducts and fibrous tissue. If you have dense breasts, you have more dense tissue than fatty tissue in your breasts. Having dense breasts can make it harder to detect breast cancer on a mammogram. If a mammogram showed that you have dense breasts, your risk of breast cancer is increased. Talk with your healthcare team about other tests you might have in addition to mammograms to look for breast cancer.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
- Having your first child at an older age. Giving birth to your first child after age 30 may increase the risk of breast cancer.
- Having never been pregnant. Having been pregnant one or more times lowers the risk of breast cancer. Never having been pregnant increases the risk.
- Inherited DNA changes that increase cancer risk. Certain DNA changes that increase the risk of breast cancer can be passed from parents to children. Two DNA changes associated with an increased risk of invasive lobular carcinoma include BRCA2 and CDH1. BRCA2 increases the risk of breast cancer and ovarian cancer. CDH1 increases the risk of breast cancer and stomach cancer. CDH1 is closely associated with a rare inherited condition called hereditary diffuse gastric cancer syndrome.
- Menopausal hormone therapy. Taking certain hormone therapy medicines to control the symptoms of menopause may increase the risk of breast cancer. The risk is linked to hormone therapy medicines that combine estrogen and progesterone. The risk goes down when you stop taking these medicines.
- Obesity. People with obesity have an increased risk of breast cancer.
- Older age. Your risk of breast cancer increases as you age. Invasive lobular carcinoma tends to happen at an older age compared to other types of breast cancer.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is higher.
Prevention
Making changes in your daily life may help lower your risk of invasive lobular carcinoma and other types of breast cancer. Try to:
Ask about breast cancer screening
Talk with your doctor or other healthcare professional about when to begin breast cancer screening. Ask about the benefits and risks of screening. Together, you can decide what breast cancer screening tests are right for you.
Become familiar with your breasts through breast self-exam
You may choose to become familiar with your breasts by occasionally inspecting them during a breast self-exam for breast awareness. If there is a new change, a lump or something not typical in your breasts, report it to a healthcare professional right away.
Breast awareness can’t prevent breast cancer. But it may help you to better understand the look and feel of your breasts. This might make it more likely that you’ll notice if something changes.
Drink alcohol in moderation, if at all
If you choose to drink alcohol, limit the amount you drink to no more than one drink a day. For breast cancer prevention, there is no safe amount of alcohol. So if you’re very concerned about your breast cancer risk, you may choose to not drink alcohol.
Exercise most days of the week
Aim for at least 30 minutes of exercise on most days of the week. If you haven’t been active lately, ask a healthcare professional whether it’s OK and start slowly.
Limit menopausal hormone therapy
Combination hormone therapy may increase the risk of breast cancer. Talk with a healthcare professional about the benefits and risks of hormone therapy.
Some people have symptoms during menopause that cause discomfort. These people may decide that the risks of hormone therapy are acceptable in order to get relief. To reduce the risk of breast cancer, use the lowest dose of hormone therapy possible for the shortest amount of time.
Maintain a healthy weight
If your weight is healthy, work to maintain that weight. If you need to lose weight, ask a healthcare professional about healthy ways to lower your weight. Eat fewer calories and slowly increase the amount of exercise.
Talk with a healthcare professional about your cancer risk
If you have a family history of breast cancer or feel that you may have an increased risk of breast cancer, talk about it with your healthcare professional. Preventive medicines, surgery and more-frequent screening may be options for people with a high risk of breast cancer.
Diagnosis
Diagnosing invasive lobular carcinoma and other kinds of breast cancer often begins with an exam and a discussion of your symptoms. Imaging tests can look at the breast tissue for anything that’s not typical. To confirm whether there is cancer or not, a sample of tissue is removed from the breast for testing.
Breast exam
During a clinical breast exam, a healthcare professional looks at the breasts for anything that’s not typical. This might include changes in the skin or to the nipple. Then the health professional feels the breasts for lumps. The health professional also feels along the collarbones and around the armpits for lumps.
Mammogram
A mammogram is an X-ray of the breast tissue. Mammograms are commonly used to screen for breast cancer. If a screening mammogram finds something concerning, you might have another mammogram to look at the area more closely. This more-detailed mammogram is called a diagnostic mammogram. It’s often used to look closely at both breasts. Invasive lobular carcinoma is less likely to be detected on a mammogram than other types of breast cancer are. Still, a mammogram is a useful diagnostic test.
Breast ultrasound
Ultrasound uses sound waves to make pictures of structures inside the body. A breast ultrasound may give your healthcare team more information about a breast lump. For example, an ultrasound might show whether the lump is a solid mass or a fluid-filled cyst. The healthcare team uses this information to decide what tests you might need next. Invasive lobular carcinoma may be more difficult to detect with ultrasound than other types of breast cancer.
Breast MRI
MRI machines use a magnetic field and radio waves to create pictures of the inside of the body. A breast MRI can make more-detailed pictures of the breast. Sometimes this method is used to look closely for any other areas of cancer in the affected breast. It also might be used to look for cancer in the other breast. Before a breast MRI, you usually receive an injection of dye. The dye helps the tissue show up better in the images.
Breast biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. To get the sample, a healthcare professional often puts a needle through the skin and into the breast tissue. The health professional guides the needle using images created with X-rays, ultrasound or another type of imaging. Once the needle reaches the right place, the health professional uses the needle to draw out tissue from the breast. Often, a marker is placed in the spot where the tissue sample was removed. The small metal marker will show up on imaging tests. The marker helps your healthcare team monitor the area of concern.
Testing cells in the lab
The tissue sample from a biopsy goes to a lab for testing. Tests can show whether the cells in the sample are cancerous. Other tests give information about the type of cancer and how quickly it’s growing. The results of these tests tell your healthcare team if you have invasive lobular carcinoma.
Special tests give more details about the cancer cells. For example, tests might look for hormone receptors on the surface of the cells. Your healthcare team uses the results from these tests to make a treatment plan.
Staging breast cancer
Once your healthcare team diagnoses your invasive lobular carcinoma, you may have other tests to figure out the extent of the cancer. This is called the cancer’s stage. Your healthcare team uses your cancer’s stage to understand your prognosis.
Complete information about your cancer’s stage may not be available until after you have breast cancer surgery.
Tests and procedures used to stage invasive lobular carcinoma may include:
- Blood tests, such as a complete blood count and tests to show how well the kidneys and liver are working.
- Bone scan.
- CT scan.
- MRI.
- Positron emission tomography scan, also called a PET scan.
Not everyone needs all of these tests. Your healthcare team picks the right tests based on your specific situation.
The stages of invasive lobular carcinoma are the same as the stages for other types of breast cancer. Breast cancer stages range from 0 to 4. A lower number means the cancer is less advanced and more likely to be cured. Stage 0 breast cancer is cancer that is contained within a breast duct. It hasn’t broken out to invade the breast tissue yet. As the cancer grows into the breast tissue and gets more advanced, the stages get higher. A stage 4 breast cancer means that the cancer has spread to other parts of the body.
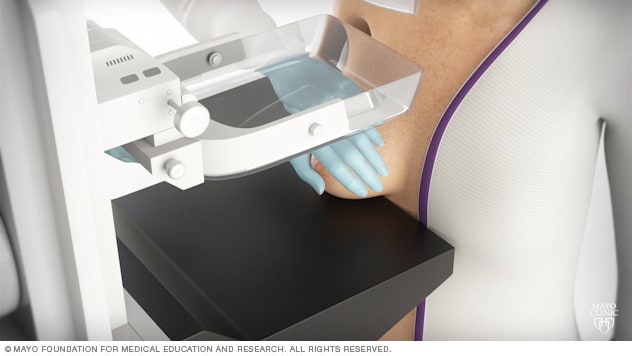
During a mammogram, you stand in front of an X-ray machine designed for mammography. A technician places your breast on a platform and positions the platform to match your height. The technician helps you position your head, arms and torso to allow an unobstructed view of your breast.
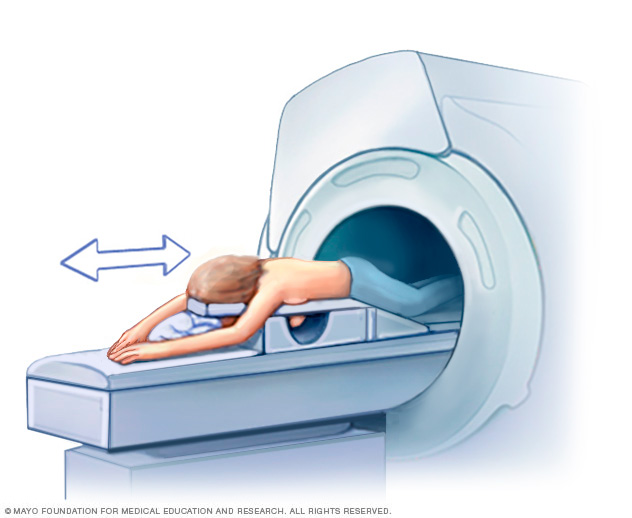
Getting a breast MRI involves lying face down on a padded scanning table. The breasts fit into a hollow space in the table. The hollow has coils that get signals from the MRI. The table slides into the large opening of the MRI machine.
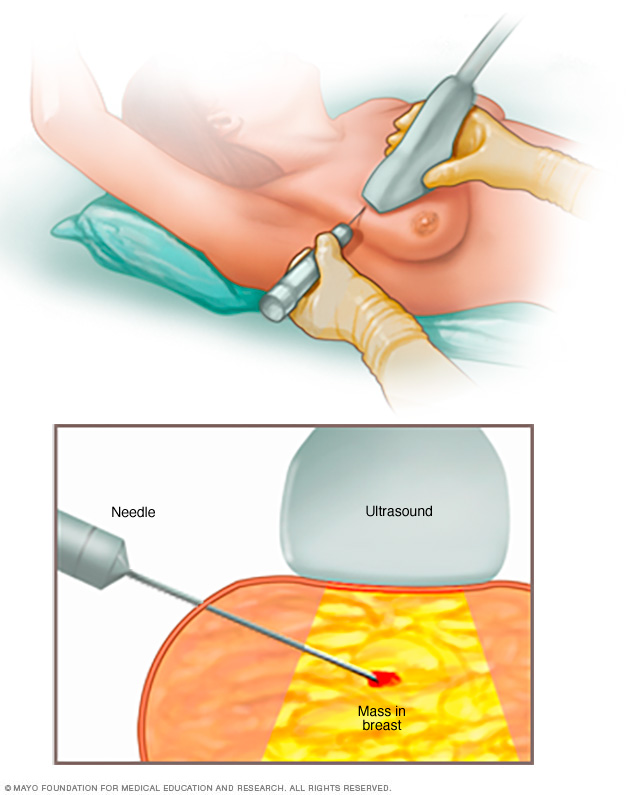
A core needle biopsy uses a long, hollow tube to obtain a sample of tissue. Here, a biopsy of a suspicious breast lump is being done. The sample is sent to a lab for testing by doctors called pathologists. They specialize in examining blood and body tissue.
Core needle biopsy Treatment
Treatment for invasive lobular carcinoma often starts with surgery to remove the cancer. Most people with breast cancer will have other treatments after surgery, such as radiation, chemotherapy and hormone therapy. Some people may have chemotherapy or hormone therapy before surgery. These medicines can help shrink the cancer and make it easier to remove.
Invasive lobular carcinoma treatment is very similar to the treatment for other types of breast cancer. Some things that might be different with this type of cancer include:
- Most invasive lobular carcinomas are sensitive to hormones. Breast cancers that are sensitive to hormones are likely to respond to hormone-blocking treatments. This kind of treatment is called hormone therapy or endocrine therapy.
- Most invasive lobular carcinomas don’t make extra HER2. HER2 is a protein that some healthy breast cells make. Some breast cancer cells develop changes that cause them to make a lot of extra HER2. Treatments can target the cells that are making extra HER2. Invasive lobular carcinomas are less likely to make extra HER2, so they’re less likely to respond to this treatment.
Your treatment plan will depend on many factors. Your healthcare team considers the stage of the cancer and how quickly it’s growing. Your care team also considers your overall health and what you prefer.
Breast cancer surgery
Surgery for invasive lobular carcinoma typically involves a procedure to remove the breast cancer and a procedure to remove some nearby lymph nodes. Options include:
-
Removing the breast cancer. A lumpectomy is surgery to remove the invasive lobular carcinoma and some of the healthy tissue around it. The rest of the breast tissue isn’t removed. Other names for this surgery are breast-conserving surgery and wide local excision. Most people who have a lumpectomy also have radiation therapy.
Lumpectomy might be used to remove a small cancer. Sometimes you can have chemotherapy before surgery to shrink the cancer so that lumpectomy is possible.
-
Removing all of the breast tissue. A mastectomy is surgery to remove all breast tissue from a breast. The most common mastectomy procedure is total mastectomy, also called simple mastectomy. This procedure removes nearly all of the breast, including the lobules, ducts, fatty tissue and some skin, including the nipple and areola.
Mastectomy might be used to remove a large invasive lobular carcinoma. It also might be needed when there are multiple areas of cancer within one breast. You might have a mastectomy if you can’t have or don’t want radiation therapy after surgery.
Some newer types of mastectomy procedures might not remove the skin or nipple. For instance, a skin-sparing mastectomy leaves some skin. A nipple-sparing mastectomy leaves the nipple and the skin around it, called the areola. These newer operations can improve the look of the breast after surgery, but they aren’t options for everyone.
- Removing a few lymph nodes. A sentinel node biopsy is an operation to take out some lymph nodes for testing. When invasive lobular carcinoma and other types of breast cancer spread, they often go to the nearby lymph nodes first. To see if the cancer has spread, a surgeon removes some of the lymph nodes near the cancer. If no cancer is found in those lymph nodes, the chance of finding cancer in any of the other lymph nodes is small. No other lymph nodes need to be removed.
- Removing several lymph nodes. Axillary lymph node dissection is an operation to remove many lymph nodes from the armpit. Your breast cancer surgery might include this operation if imaging tests show the cancer has spread to the lymph nodes. It also might be used if cancer is found in a sentinel node biopsy.
- Removing both breasts. Some people who have invasive lobular carcinoma in one breast may choose to have their other breast removed, even if it doesn’t have cancer. This procedure is called a contralateral prophylactic mastectomy or a risk-reducing mastectomy. It might be an option if you have a high risk of getting cancer in the other breast. The risk might be high if you have a strong family history of cancer or have DNA changes that increase the risk of cancer. Most people with breast cancer in one breast will never get cancer in the other breast.
Complications of breast cancer surgery depend on the procedures you choose. All operations have a risk of pain, bleeding and infection. Removing lymph nodes in the armpit carries a risk of arm swelling, called lymphedema.
You may choose to have breast reconstruction after mastectomy surgery. Breast reconstruction is surgery to restore shape to the breast. Options might include reconstruction with a breast implant or reconstruction using your own tissue. Consider asking your healthcare team for a referral to a plastic surgeon before your breast cancer surgery.
Hormone therapy
Hormone therapy, also called endocrine therapy, uses medicines to block certain hormones in the body. It’s a treatment for breast cancers that are sensitive to the hormones estrogen and progesterone. Healthcare professionals call these cancers estrogen receptor positive and progesterone receptor positive. Cancers that are sensitive to hormones use the hormones as fuel for their growth. Blocking the hormones can cause the cancer cells to shrink or die. Most invasive lobular carcinomas are sensitive to hormones, so they are likely to respond to this treatment.
Hormone therapy is often used after surgery and other treatments. It can lower the risk that the cancer will come back.
If the invasive lobular carcinoma spreads to other parts of the body, hormone therapy can help control it.
Treatments that can be used in hormone therapy include:
- Medicines that block hormones from attaching to cancer cells. These medicines are called selective estrogen receptor modulators.
- Medicines that stop the body from making estrogen after menopause. These medicines are called aromatase inhibitors.
- Surgery or medicines to stop the ovaries from making hormones.
Sometimes hormone therapy medicines are combined with targeted therapy medicines. This combination can make hormone therapy more effective.
Hormone therapy side effects depend on the treatment you receive. The side effects can include hot flashes, night sweats and vaginal dryness. More-serious side effects include a risk of bone thinning and blood clots.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources.
The radiation used to treat invasive lobular carcinoma and other types of breast cancer is often external beam radiation. During this type of radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Less often, the radiation can be placed inside the body. This type of radiation is called brachytherapy.
Radiation therapy is often used after surgery. It can kill any cancer cells that might be left after surgery. The radiation lowers the risk of the cancer coming back.
Side effects of radiation therapy include feeling very tired and having a sunburn-like rash where the radiation is aimed. Breast tissue also may look swollen or feel more firm. Rarely, more-serious side effects can happen. These include damage to the heart or lungs. Very rarely, a new cancer can grow in the treated area.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Treatment often involves a combination of chemotherapy medicines. Most are given through a vein. Some are available in pill form.
Chemotherapy for invasive lobular carcinoma and other types of breast cancer is often used after surgery. It can kill any cancer cells that might remain and lower the risk of the cancer coming back.
Sometimes chemotherapy is given before surgery for invasive lobular carcinoma and other types of breast cancer. The chemotherapy might shrink the breast cancer so that it’s easier to remove. Chemotherapy before surgery also might control cancer that spreads to the lymph nodes. If the lymph nodes no longer show signs of cancer after chemotherapy, surgery to remove many lymph nodes might not be needed. How the cancer responds to chemotherapy before surgery helps the healthcare team make decisions about what treatments might be needed after surgery.
When the cancer spreads to other parts of the body, chemotherapy can help control it. Chemotherapy may relieve symptoms of an advanced cancer, such as pain.
Chemotherapy side effects depend on which medicines you receive. Common side effects include hair loss, nausea, vomiting, feeling very tired and having an increased risk of getting an infection. Rare side effects can include premature menopause and nerve damage. Very rarely, certain chemotherapy medicines can cause blood cell cancer.
Targeted therapy
Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
The most common targeted therapy medicines for breast cancer target the protein HER2. Some breast cancer cells make extra HER2. This protein helps the cancer cells grow and survive. Targeted therapy medicine attacks the cells that are making extra HER2 and doesn’t hurt healthy cells. Most invasive lobular carcinomas don’t make extra HER2, so they are unlikely to respond to treatments that target HER2.
Many other targeted therapy medicines exist for treating breast cancer. Your cancer cells may be tested to see whether these medicines might help you.
Targeted therapy medicines can be used before surgery to shrink a breast cancer and make it easier to remove. Some are used after surgery to lower the risk that the cancer will come back. Others are used only when the cancer has spread to other parts of the body.
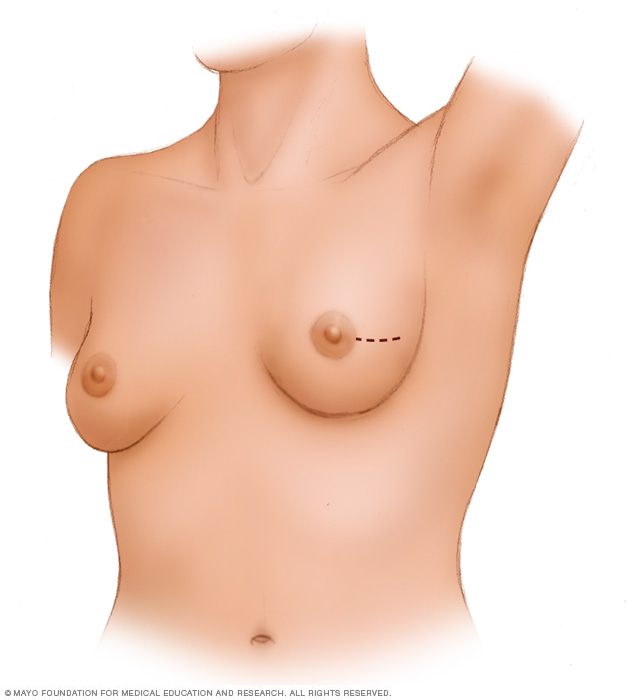
A lumpectomy involves removing the cancer and some of the healthy tissue that surrounds it. This illustration shows one possible incision that can be used for this procedure, though your surgeon will determine the approach that’s best for your particular situation.
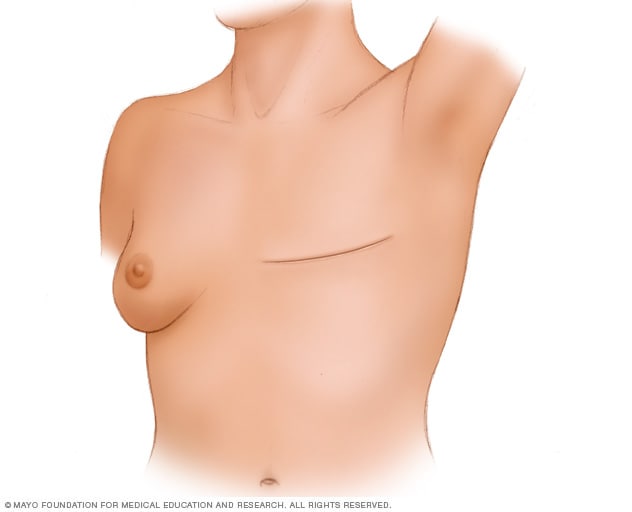
During a total mastectomy, the surgeon removes the breast tissue, nipple, areola and skin. This procedure also is known as a simple mastectomy. Other mastectomy procedures may leave some parts of the breast, such as the skin or the nipple. Surgery to create a new breast is optional. It may be done at the same time as mastectomy surgery or it can be done later.
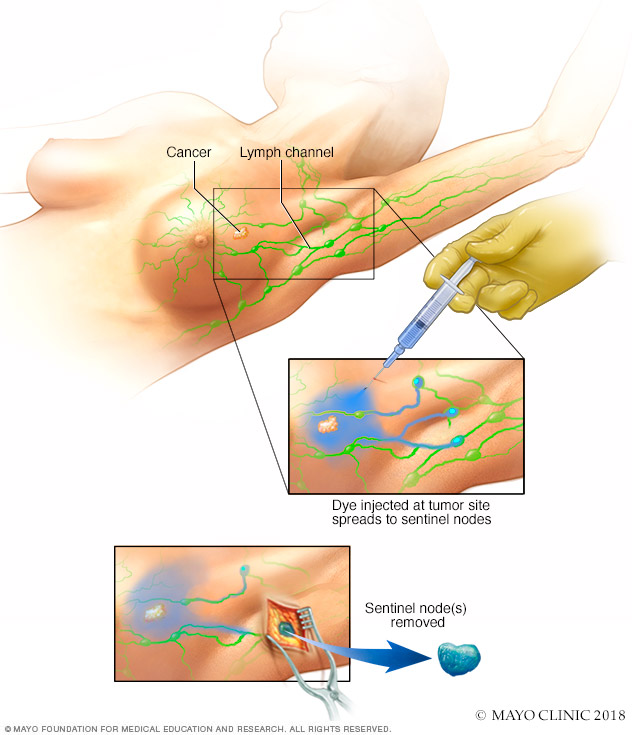
Sentinel node biopsy identifies the first few lymph nodes into which a tumor drains. The surgeon uses a harmless dye and a weak radioactive solution to locate the sentinel nodes. The nodes are removed and tested for signs of cancer.
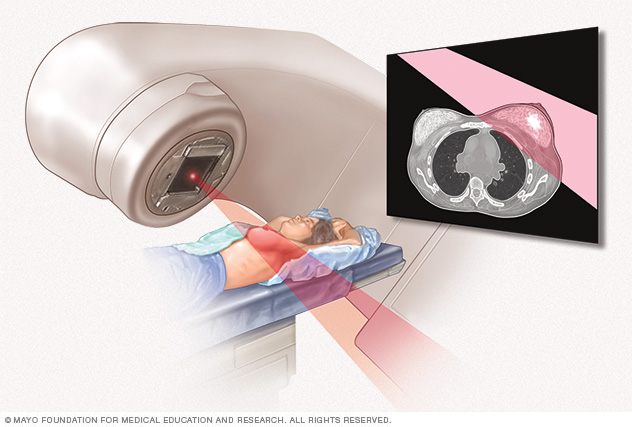
External beam radiation uses high-powered beams of energy to kill cancer cells. Beams of radiation are precisely aimed at the cancer using a machine that moves around your body.
Radiation therapy Alternative medicine
No alternative medicine treatments have been found to cure invasive lobular carcinoma or other types of breast cancer. But complementary and alternative medicine therapies may help you cope with the side effects of treatment.
Alternative treatments for hot flashes
Hot flashes are bouts of sudden, intense warmness that can leave you sweaty and uncomfortable. They can be a symptom of natural menopause or a side effect of hormone therapy for breast cancer. Hormone therapy, also called endocrine therapy, is often used to treat invasive lobular carcinoma.
Talk to your healthcare professional if you experience hot flashes. Many conventional treatments are available for hot flashes, including medicines.
If treatments for hot flashes don’t work as well as you’d like, it might help to add complementary and alternative treatments to help you feel better.
Options might include:
- Acupuncture.
- Hypnosis.
- Meditation.
- Relaxation techniques.
- Tai chi.
- Yoga.
While none of these alternative treatments are proved to help control hot flashes, evidence shows that some breast cancer survivors find them helpful.
If you’re interested in trying alternative treatments for hot flashes, talk to your healthcare team about your options.
Coping and support
Some breast cancer survivors say their diagnosis felt overwhelming at first. It can be stressful to feel overwhelmed right when you need to make important decisions about your treatment. In time, you’ll find ways to cope with your feelings. Until you find what works for you, it might help to:
Learn enough about invasive lobular carcinoma to make decisions about your care
If you’d like to know more about your cancer, ask your healthcare team for the details. Write down the type, stage and hormone receptor status. Ask for good sources of information where you can learn more about your treatment options.
Knowing more about your cancer and your options may help you feel more confident when making treatment decisions. Still, some people don’t want to know the details of their cancer. If this is how you feel, let your care team know that too.
Keep your friends and family close
Your friends and family can provide a crucial support network for you during your cancer treatment.
As you begin telling people about your breast cancer diagnosis, you’ll likely get many offers for help. Think ahead about things you may want help with. Examples include listening when you want to talk or helping you with preparing meals.
Connect with other people with cancer
You may find it helpful and encouraging to talk to others who have been diagnosed with breast cancer. Contact a cancer support organization in your area to find out about support groups near you or online. In the United States, you might start with the American Cancer Society.
Find someone to talk with about your feelings
Find a friend or family member who is a good listener. Or talk with a clergy member or counselor. Ask your healthcare team for a referral to a counselor or other professional who works with people who have cancer.
Take care of yourself
During your treatment, allow yourself time to rest. Take good care of your body by getting enough sleep so that you wake feeling rested and by taking time to relax. Choose a diet full of fruits and vegetables and stay as physically active as you’re able. Try to maintain at least some of your daily routine, including social activities.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If an exam or imaging test shows you might have invasive lobular carcinoma, your healthcare team will likely refer you to a specialist.
Specialists who care for people with breast cancer include:
- Breast health specialists.
- Breast surgeons.
- Doctors who specialize in diagnostic tests, such as mammograms, called radiologists.
- Doctors who specialize in treating cancer, called oncologists.
- Doctors who treat cancer with radiation, called radiation oncologists.
- Genetic counselors.
- Plastic surgeons.
What you can do to prepare
- Write down any symptoms you’re experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Write down your family history of cancer. Note any family members who have had cancer. Note how each member is related to you, the type of cancer, the age at diagnosis and whether each person survived.
- Make a list of all medicines, vitamins or supplements that you’re taking.
- Keep all of your records that relate to your cancer diagnosis and treatment. Organize your records in a binder or folder that you can take to your appointments.
- Consider taking a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
Your time with your healthcare professional is limited. Prepare a list of questions so that you can make the most of your time together. List your questions from most important to least important in case time runs out. For invasive lobular carcinoma, some basic questions to ask include:
- Do I have breast cancer?
- What is the size of my breast cancer?
- What is the stage of my breast cancer?
- Will I need additional tests?
- How will those tests help you determine the best treatments for me?
- What are the treatment options for my cancer?
- What are the side effects of each treatment option?
- How will each treatment option affect my daily life? Can I continue working?
- Is there one treatment you recommend over the others?
- How do you know that these treatments will benefit me?
- What would you recommend to a friend or family member in my situation?
- How quickly do I need to make a decision about cancer treatment?
- What happens if I don’t want cancer treatment?
- What will cancer treatment cost?
- Does my insurance plan cover the tests and treatment you’re recommending?
- Should I seek a second opinion? Will my insurance cover it?
- Are there any brochures or other printed material that I can take with me? What websites or books do you recommend?
In addition to the questions that you’ve prepared, don’t hesitate to ask other questions you think of during your appointment.
What to expect from your doctor
Be prepared to answer some questions about your symptoms and your health, such as:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



