Nephrotic syndrome
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Swelling around your feet and ankles is a common sign of this condition that occurs when your kidneys pass too much protein in your urine.
Overview
, Overview, ,
Nephrotic syndrome is a kidney disorder that causes your body to pass too much protein in your urine.
Nephrotic syndrome is usually caused by damage to the clusters of small blood vessels in your kidneys that filter waste and excess water from your blood. The condition causes swelling, particularly in your feet and ankles, and increases the risk of other health problems.
Treatment for nephrotic syndrome includes treating the condition that’s causing it and taking medications. Nephrotic syndrome can increase your risk of infections and blood clots. Your doctor might recommend medications and dietary changes to prevent complications.
Signs and symptoms of nephrotic syndrome include:
- Severe swelling (edema), particularly around your eyes and in your ankles and feet
- Foamy urine, a result of excess protein in your urine
- Weight gain due to fluid retention
- Fatigue
- Loss of appetite
When to see a doctor
Make an appointment with your doctor if you have signs or symptoms that worry you.
Causes
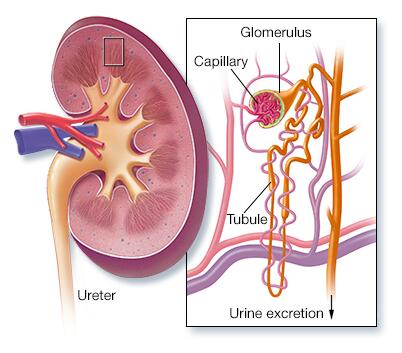
Nephrotic syndrome is usually caused by damage to the clusters of tiny blood vessels (glomeruli) of your kidneys.
The glomeruli filter your blood as it passes through your kidneys, separating things your body needs from those it doesn’t. Healthy glomeruli keep blood protein (mainly albumin) — which is needed to maintain the right amount of fluid in your body — from seeping into your urine. When damaged, glomeruli allow too much blood protein to leave your body, leading to nephrotic syndrome.
Many possible causes
Many diseases and conditions can cause glomerular damage and lead to nephrotic syndrome, including:
- Diabetic kidney disease. Diabetes can lead to kidney damage (diabetic nephropathy) that affects the glomeruli.
- Minimal change disease. This is the most common cause of nephrotic syndrome in children. Minimal change disease results in abnormal kidney function, but when the kidney tissue is examined under a microscope, it appears normal or nearly normal. The cause of the abnormal function typically can’t be determined.
- Focal segmental glomerulosclerosis. Characterized by scarring of some of the glomeruli, this condition can result from another disease, a genetic defect or certain medications or occur for no known reason.
- Membranous nephropathy. This kidney disorder is the result of thickening membranes within the glomeruli. The thickening is due to deposits made by the immune system. It can be associated with other medical conditions, such as lupus, hepatitis B, malaria and cancer, or it can occur for no known reason.
- Systemic lupus erythematosus. This chronic inflammatory disease can lead to serious kidney damage.
- Amyloidosis. This disorder occurs when amyloid proteins accumulate in your organs. Amyloid buildup often damages the kidneys’ filtering system.
Risk factors
Factors that can increase your risk of nephrotic syndrome include:
- Medical conditions that can damage your kidneys. Certain diseases and conditions increase your risk of developing nephrotic syndrome, such as diabetes, lupus, amyloidosis, reflux nephropathy and other kidney diseases.
- Certain medications. Medications that might cause nephrotic syndrome include nonsteroidal anti-inflammatory drugs and drugs used to fight infections.
- Certain infections. Infections that increase the risk of nephrotic syndrome include HIV, hepatitis B, hepatitis C and malaria.
Complications
Possible complications of nephrotic syndrome include:
- Blood clots. The inability of the glomeruli to filter blood properly can lead to loss of blood proteins that help prevent clotting. This increases your risk of developing a blood clot in your veins.
- High blood cholesterol and elevated blood triglycerides. When the level of the protein albumin in your blood falls, your liver makes more albumin. At the same time, your liver releases more cholesterol and triglycerides.
- Poor nutrition. Loss of too much blood protein can result in malnutrition. This can lead to weight loss, which can be masked by edema. You may also have too few red blood cells (anemia), low blood protein levels and low levels of vitamin D.
- High blood pressure. Damage to your glomeruli and the resulting buildup of excess body fluid can raise your blood pressure.
- Acute kidney injury. If your kidneys lose their ability to filter blood due to damage to the glomeruli, waste products can build up quickly in your blood. If this happens, you might need emergency dialysis — an artificial means of removing extra fluids and waste from your blood — typically with an artificial kidney machine (dialyzer).
- Chronic kidney disease. Nephrotic syndrome can cause your kidneys to lose their function over time. If kidney function falls low enough, you might need dialysis or a kidney transplant.
- Infections. People with nephrotic syndrome have an increased risk of infections.
Diagnosis
Tests and procedures used to diagnose nephrotic syndrome include:
- Urine tests. A urinalysis can reveal abnormalities in your urine, such as large amounts of protein. You might be asked to collect urine samples over 24 hours.
- Blood tests. A blood test can show low levels of the protein albumin and often decreased levels of blood protein overall. Loss of albumin is often associated with an increase in blood cholesterol and blood triglycerides. The creatinine and urea nitrogen levels in your blood also might be measured to assess your overall kidney function.
- Kidney biopsy. Your doctor might recommend removing a small sample of kidney tissue for testing. During a kidney biopsy, a needle is inserted through your skin and into your kidney. Kidney tissue is collected and sent to a lab for testing.
Treatment
Treatment for nephrotic syndrome involves treating any medical condition that might be causing your nephrotic syndrome. Your doctor might also recommend medications and changes in your diet to help control your signs and symptoms or treat complications of nephrotic syndrome.
Medications might include:
-
Blood pressure medications. Drugs called angiotensin-converting enzyme (ACE) inhibitors reduce blood pressure and the amount of protein released in urine. Medications in this category include lisinopril (Prinivil, Qbrelis, Zestril), benazepril (Lotensin), captopril and enalapril (Vasotec).
Another group of drugs that works similarly is called angiotensin II receptor blockers (ARBs) and includes losartan (Cozaar) and valsartan (Diovan). Other medications, such as renin inhibitors, also might be used, though ACE inhibitors and ARBs are generally used first.
- Water pills (diuretics). These help control swelling by increasing your kidneys’ fluid output. Diuretic medications typically include furosemide (Lasix). Others include spironolactone (Aldactone, Carospir) and thiazides, such as hydrochlorothiazide or metolazone (Zaroxolyn).
-
Cholesterol-reducing medications. Statins can help lower cholesterol levels. However, it’s not clear whether cholesterol-lowering medications can improve the outcomes for people with nephrotic syndrome, such as avoiding heart attacks or decreasing the risk of early death.
Statins include atorvastatin (Lipitor), fluvastatin (Lescol XL), lovastatin (Altoprev), pravastatin (Pravachol), rosuvastatin (Crestor, Ezallor) and simvastatin (Zocor).
- Blood thinners (anticoagulants). These might be prescribed to decrease your blood’s ability to clot, especially if you’ve had a blood clot. Anticoagulants include heparin, warfarin (Coumadin, Jantoven), dabigatran (Pradaxa), apixaban (Eliquis) and rivaroxaban (Xarelto).
- Immune system-suppressing medications. Medications to control the immune system, such as corticosteroids, can decrease the inflammation that accompanies some of the conditions that can cause nephrotic syndrome. Medications include rituximab (Rituxan), cyclosporine and cyclophosphamide.
Self care
Changes to your diet might help with nephrotic syndrome. Your doctor might refer you to a dietitian, who might recommend that you do the following:
- Choose lean sources of protein. Plant-based protein is helpful in kidney disease.
- Reduce the amount of fat and cholesterol in your diet to help control your blood cholesterol levels.
- Eat a low-salt diet to help control swelling.
- Reduce the amount of liquid in your diet.
Preparing for your appointment
Start by seeing your primary care doctor. If your doctor suspects you or your child has a kidney problem, such as nephrotic syndrome, you might be referred to a doctor who specializes in the kidneys (nephrologist).
Here’s some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there’s anything you need to do in advance, such as restrict your diet. Take a family member or friend along, if possible, to help you remember the information you’ll be given.
Make a list of:
- Your or your child’s symptoms and when they began
- Key personal information, including major stresses or recent life changes
- All medications, vitamins or other supplements you or your child takes, including doses
- Questions to ask your doctor
For nephrotic syndrome, some questions to ask include:
- What’s the most likely cause of my or my child’s nephrotic syndrome?
- What tests do I or my child need?
- Is this condition likely temporary?
- What are the treatment options? And which do you recommend?
- Are there changes I can make to my or my child’s diet? Could consulting a dietitian help?
- How can I best manage this condition with my or my child’s other medical conditions?
- Are there brochures or other printed material that I can have? What websites do you recommend?
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- Do symptoms come and go, or do you have them all the time?
- How severe are the symptoms?
- Does anything seem to improve the symptoms?
- What, if anything, appears to worsen the symptoms?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



