Prolactinoma
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Learn how this pituitary gland tumor alters certain hormone levels and leads to problems such as infertility, decreased libido and vision problems.
Overview
, Overview, ,
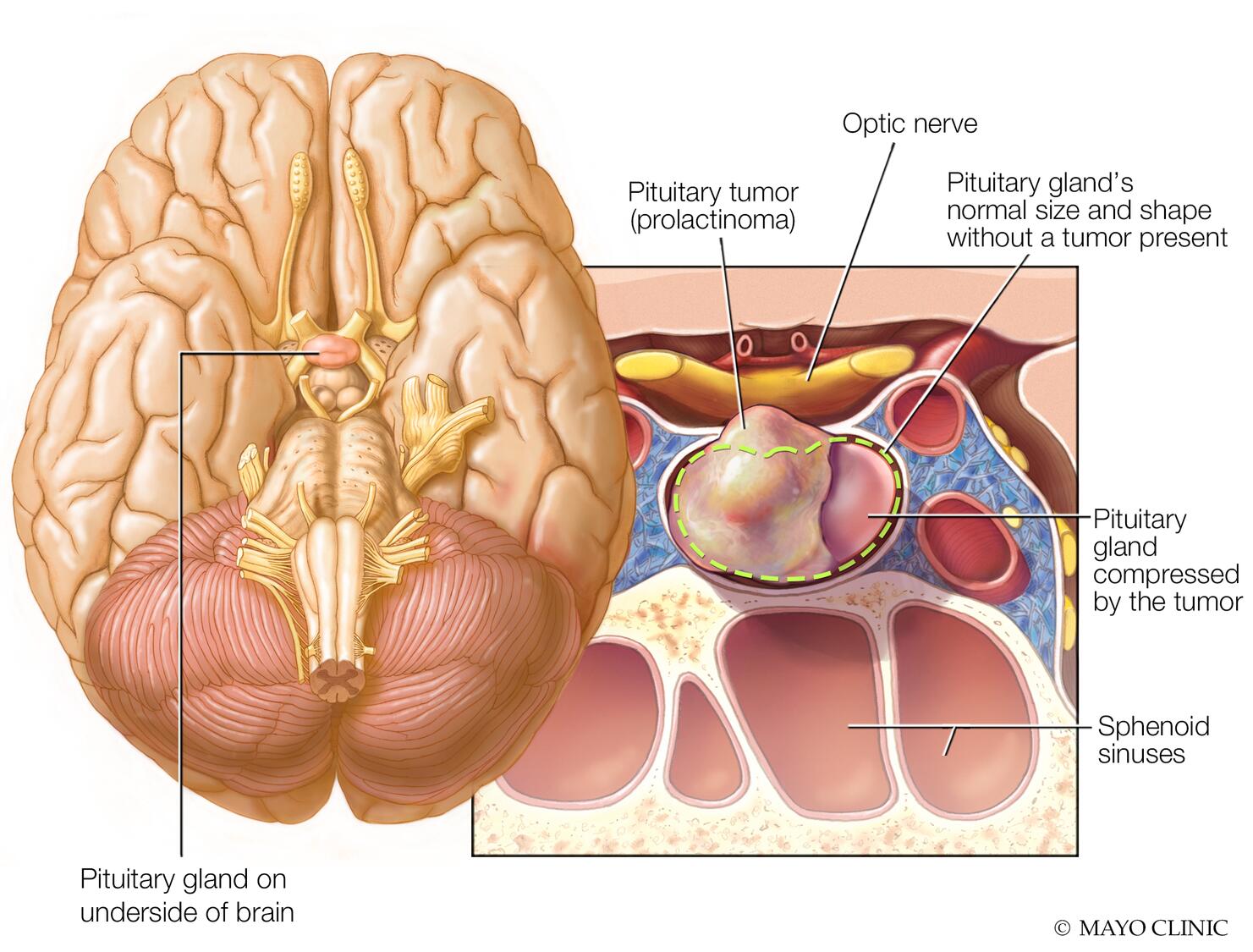
Prolactinoma is a noncancerous tumor of the pituitary gland. This tumor causes the pituitary gland to make too much of a hormone called prolactin. The major effect of a prolactinoma is decreased levels of some sex hormones — namely, estrogen and testosterone.
A prolactinoma isn’t life-threatening. But it can cause vision difficulties, infertility and other problems. Prolactinoma is the most common type of hormone-producing tumor that can develop in the pituitary gland.
A prolactinoma can usually be treated with medications to bring the prolactin level down into the standard range and shrink the tumor. In some cases, surgery to remove the tumor might be an option.
A prolactinoma might not cause any signs or symptoms. However, too much prolactin in your blood (hyperprolactinemia) can cause symptoms. So can pressure on surrounding tissues from a large tumor.
Because too much prolactin can disrupt the reproductive system (hypogonadism), some of the signs and symptoms of a prolactinoma are specific to females or males.
In females, prolactinoma can cause:
- Irregular menstrual periods or no menstrual periods
- Milky discharge from the breasts when not pregnant or breastfeeding
- Painful intercourse due to vaginal dryness
- Acne and excessive body and facial hair growth
In males, prolactinoma can cause:
- Erectile dysfunction
- Decreased body and facial hair
- Smaller muscles
- Enlarged breasts
In both females and males, prolactinoma can cause:
- Infertility
- Weak and brittle bones that break easily (osteoporosis)
- Loss of interest in sexual activity
Pressure from tumor growth can cause:
- Vision problems
- Headache
- Reduction of other hormones produced by the pituitary gland
Females who are premenopausal tend to notice signs and symptoms early, when tumors are smaller in size. This is probably because of missed or irregular menstrual periods. Females who are postmenopausal are more likely to notice signs and symptoms later, when tumors are larger and more likely to cause headache or vision problems. Males are also more likely to notice signs and symptoms later.
When to see a doctor
If you develop signs and symptoms that may be caused by a prolactinoma, see your health care provider to determine the cause.
If you have a prolactinoma and you want to become or are already pregnant, talk to your health care provider. Adjustments in your treatment and monitoring may be necessary.
Causes
Prolactinoma is one type of tumor that develops in the pituitary gland. The cause of prolactinoma is usually unknown.
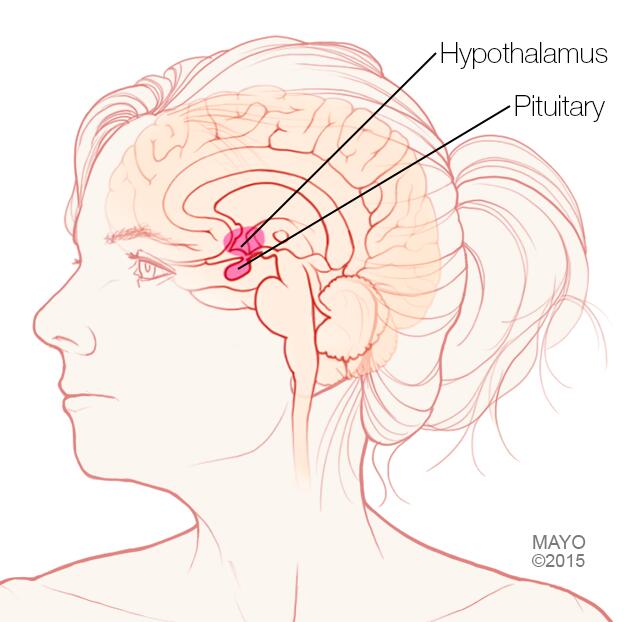
The pituitary gland is a small bean-shaped gland located at the base of your brain. Despite its small size, the pituitary gland has an effect on nearly every part of your body. Its hormones help control important functions such as growth, metabolism, blood pressure and reproduction.
A prolactinoma causes the pituitary gland to make too much of a hormone called prolactin. This results in a decreased level of some sex hormones — namely, estrogen and testosterone.
Making too much prolactin (hyperprolactinemia) can also happen for reasons other than a prolactinoma. These can include:
- Medications
- Other types of pituitary tumors
- Kidney disease
- Underactive thyroid gland
- Pregnancy and breastfeeding
More prolactinomas occur in females than males. The disorder is rare in children.
Rarely, an inherited disorder such as multiple endocrine neoplasia, type 1 — a disorder that causes tumors in hormone-producing glands — may increase the risk of a prolactinoma.
Complications
Complications of prolactinoma may include:
- Infertility. A prolactinoma can interfere with reproduction. Too much prolactin reduces the production of the hormones estrogen and testosterone. Too much prolactin also can prevent the release of an egg during the menstrual cycle (anovulation) in females. In males, too much prolactin also can lead to decreased sperm production.
- Bone loss (osteoporosis). Reduced estrogen and testosterone also cause decreased bone strength. This results in weak and brittle bones that can break easily.
- Pregnancy complications. During a typical pregnancy, the production of estrogen increases. This may cause tumor growth. This can result in signs and symptoms such as headaches and changes in vision in pregnant females who have large prolactinomas.
- Vision loss. Left untreated, a prolactinoma may grow large enough to press on your optic nerve. This nerve sits near the pituitary gland. The nerve sends images from your eye to your brain so that you can see. The first sign of pressure on the optic nerve is a loss of your side (peripheral) vision.
- Low levels of other pituitary gland hormones. Larger prolactinomas can put pressure on the healthy part of the pituitary gland. This can lead to lower levels of other hormones controlled by the pituitary gland. These include thyroid hormones and cortisol. Cortisol is a stress-response hormone.
Diagnosis
If you have signs and symptoms that suggest you have a prolactinoma, your health care provider may recommend:
- Blood tests. Blood tests can show if too much prolactin is being made. They can also show whether levels of other hormones controlled by the pituitary gland are within the standard range. A pregnancy test is typically recommended for females of childbearing age.
- Brain imaging. Your provider may be able to detect a prolactinoma using a magnetic resonance imaging (MRI) scan of your brain.
- Vision tests. These can determine if a prolactinoma is affecting your sight.
Your provider may also refer you for additional testing with a specialist in treating disorders that affect the endocrine glands and hormones (endocrinologist).
Treatment
Goals in the treatment of a prolactinoma include:
- Return the production of prolactin to within the standard range
- Reduce the size of the prolactinoma
- Restore healthy pituitary gland function
For most people, treatment can eliminate or improve:
- Problems caused by increased prolactin levels, such as irregular menstrual periods, infertility and loss of interest in sexual activity
- Signs or symptoms from tumor pressure, such as headaches or vision problems
Prolactinoma treatment includes two main therapies: medications and surgery.
Medications
Oral medications known as dopamine agonists are generally used to treat a prolactinoma. These drugs mimic the effects of dopamine — the brain chemical that controls how much prolactin is made. Dopamine agonists can decrease the production of prolactin and shrink the size of the tumor. Drugs can eliminate symptoms for most people with prolactinomas. However, you’ll generally need long-term treatment with drugs.
Commonly prescribed drugs include cabergoline and bromocriptine (Cycloset, Parlodel).
If a drug shrinks the tumor significantly and your prolactin level remains within the standard range for two years, you may be able to taper off the drug. Only taper off your drug with your health care provider’s guidance. Your provider monitors your prolactin levels during this process. Don’t stop taking your drug without talking to your provider first.
Prolactin levels commonly rise after stopping the drug. If this happens, your provider will likely ask you to restart taking the drug.
Common medication side effects
Common side effects of these medications include nausea and vomiting, dizziness, nasal stuffiness, and headache. However, these side effects often can be less bothersome if your health care provider starts you with a very low dose of the drug. Then your provider can gradually increase the dose. It may also help if you take the drug with food or if you take it at bedtime.
People have rarely had heart valve damage with cabergoline. But it’s usually in people taking much higher doses for Parkinson’s disease. Some people may develop impulse control disorders, such as compulsive gambling, while taking these drugs.
Medication during pregnancy
Both bromocriptine and cabergoline treat prolactinomas in people who want to become pregnant. But the medications have different advantages and disadvantages. Discuss the pros and cons of these options with your health care provider. Together you can decide which drug may work best for you.
In most situations, a provider typically advises stopping the drug when pregnancy is confirmed. Although both drugs are considered safe in pregnancy, your provider will generally recommend avoiding any drug during pregnancy when possible. However, if you have a large prolactinoma or you develop signs and symptoms such as headaches or vision changes, your provider may recommend that you restart the drug. This can prevent further tumor growth and complications.
If you’re being treated for a prolactinoma and you’d like to start a family, it’s best to discuss your options with your provider before you become pregnant.
Surgery
Surgery to remove a prolactinoma is generally an option if drug therapy doesn’t work or you can’t tolerate the drug. Surgery may be necessary to relieve pressure on the nerves that control your vision.
The type of surgery you have will depend largely on the size and extent of your tumor:
- Nasal surgery. For most people who need surgery, the procedure involves removing the tumor through the nose (nasal cavity). This surgery is called transsphenoidal surgery. Complication rates are low because the surgeon doesn’t touch other areas of the brain during surgery. This surgery leaves no visible scars.
- Transcranial surgery. If your tumor is large or has extended to nearby brain tissue, you may need this procedure, also known as a craniotomy. The surgeon removes the tumor through the upper part of the skull.
Surgery outcomes depend on the size and location of the tumor and prolactin levels before surgery. The surgeon’s skill and experience with this specific type of surgery also is a factor. Sometimes an MRI scan shows that a prolactinoma has extended to areas in the brain where it’s unsafe to attempt removal. When this happens, the surgeon can only partially remove the prolactinoma.
Surgery corrects the prolactin level in most people with small prolactinomas. However, tumors may come back within several years of surgery. For people with larger tumors that can only be partially removed, drug therapy often can return the prolactin level to the standard range after surgery.
Radiation
Rarely, radiation therapy to kill tumor cells may be an option for a large prolactinoma. You may have radiation if you don’t respond to medication, if you aren’t able to have surgery, or if your surgery didn’t remove all of a large tumor.
Preparing for your appointment
You’ll likely start by seeing your family health care provider. You may then be referred to a specialist in disorders that affect the endocrine glands and hormones (endocrinologist).
Here’s some information to help you get ready for your appointment.
What you can do
Before your appointment, you may want to make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment
- Your menstrual history, including age at onset of periods, episodes of missed menstrual periods, approximate dates and type of contraceptives used
- Key personal information, including major stresses or recent life changes
- All medications, vitamins, herbs and supplements you’re taking, and the dosages
- Questions for your health care provider
Basic questions to ask may include:
- What’s the most likely cause of my symptoms?
- What are other possible causes?
- What tests do I need? Do they require special preparation?
- What treatments are available, and which do you recommend?
- What side effects can I expect from treatment?
- If I have surgery, will the prolactinoma come back?
- I have other health conditions. How can I best manage them together?
- Will I be able to have children?
- Is there a generic alternative to the medication you’re prescribing?
- Are there brochures or other printed material that I can take? What websites do you recommend?
Don’t hesitate to ask any other questions during your appointment.
What to expect from your doctor
Your provider is likely to ask you questions, including:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you or family members ever had high calcium levels, kidney stones or tumors in endocrine glands?
Preparing to answer questions can help you make the most of your appointment time.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



