Spermatocele
![]() August, 10th, 2023
August, 10th, 2023
Benefit Summary
Learn more about this noncancerous testicular disorder that may require surgery if it’s causing discomfort. But, the condition often needs no treatment.
Overview
, Overview, ,
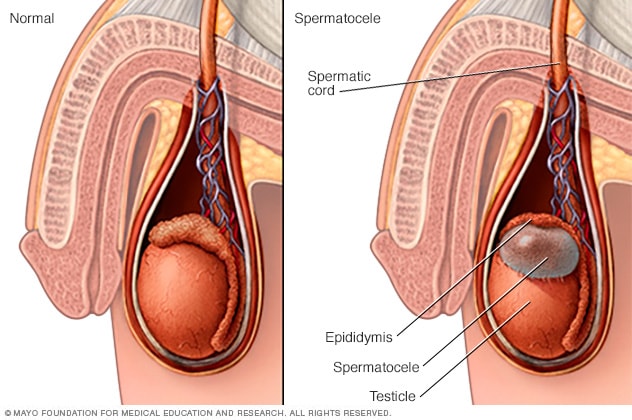
A spermatocele (SPUR-muh-toe-seel) is an abnormal sac (cyst) that develops in the epididymis — the small, coiled tube located on the upper testicle that collects and transports sperm. Noncancerous and generally painless, a spermatocele usually is filled with milky or clear fluid that might contain sperm.
The exact cause of spermatoceles isn’t clear, but they might be due to a blockage in one of the tubes that transport sperm.
Spermatoceles, sometimes called spermatic cysts, are common. They typically don’t reduce fertility or require treatment. If a spermatocele grows large enough to cause discomfort, your doctor might suggest surgery.
A spermatocele usually causes no signs or symptoms and might remain stable in size. If it becomes large enough, however, you might feel:
- Pain or discomfort in the affected testicle
- Heaviness in the testicle with the spermatocele
- Fullness behind and above the testicle
When to see a doctor
Because a spermatocele usually doesn’t cause symptoms, you might discover it only during a testicular self-exam, or your doctor might find it during a routine physical exam.
It’s a good idea to have your doctor evaluate any scrotal mass to rule out a serious condition, such as testicular cancer. Also, call your doctor if you experience pain or swelling in your scrotum. A number of conditions can cause testicular pain, and some require immediate treatment.
Causes
The cause of spermatoceles is unknown. Spermatoceles might result from a blockage in one of the multiple tubes within the epididymis that transport and store sperm from the testicle.
Risk factors
There aren’t many known risk factors for developing a spermatocele. Men whose mothers were given the drug diethylstilbestrol (DES) during pregnancy to prevent miscarriage and other pregnancy complications appear to have a higher risk of spermatoceles. Use of this drug was stopped in 1971 due to concerns about an increased risk of rare vaginal cancer in women.
Complications
A spermatocele is unlikely to cause complications.
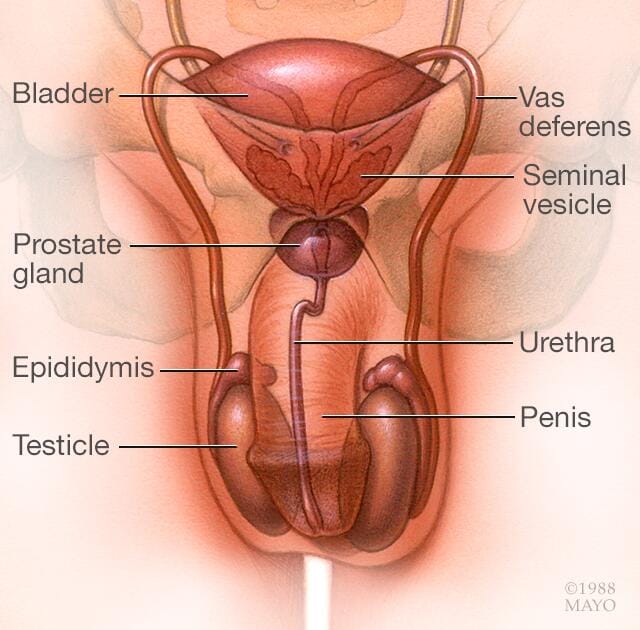
However, if your spermatocele is painful or has grown so large that it’s causing you discomfort, you might need to have surgery to remove the spermatocele. Surgical removal might damage the epididymis or the vas deferens, a tube that transports sperm from the epididymis to the penis. Damage to either can reduce fertility. Another possible complication that can occur after surgery is that the spermatocele might come back, though this is uncommon.
Although there’s no way to prevent a spermatocele, it’s important for you to conduct scrotal self-exams at least monthly to detect changes, such as masses, in your scrotum. Any new mass in your scrotum should be evaluated promptly.
Your doctor can instruct you in how to conduct a testicular self-examination, which can improve your chances of finding a mass.
How to examine your testicles
A good time to examine your testicles is during or after a warm bath or shower. The heat from the water relaxes your scrotum, making it easier for you to detect anything unusual. Then follow these steps:
- Stand in front of a mirror. Look for any swelling on the skin of the scrotum.
- Examine each testicle with both hands. Place the index and middle fingers under the testicle while placing your thumbs on the top.
- Gently roll the testicle between the thumbs and the fingers. Remember that the testicles are usually smooth, oval shaped and somewhat firm. It’s normal for one testicle to be slightly larger than the other. Also, the cord leading upward from the top of the testicle (epididymis) is a normal part of the scrotum.
By regularly performing this exam, you’ll become more familiar with your testicles and aware of any changes that might be of concern. If you find a lump, call your doctor as soon as possible.
Regular self-examination is an important health habit. But it can’t substitute for a doctor’s examination. Your doctor normally checks your testicles whenever you have a physical exam.
Diagnosis
To diagnose a spermatocele, you’ll need a physical exam. Although a spermatocele generally isn’t painful, you might feel discomfort when your doctor examines (palpates) the mass.
You might also undergo the following diagnostic tests:
- Transillumination. Your doctor might shine a light through your scrotum. With a spermatocele, the light will indicate that the mass is fluid-filled rather than solid.
- Ultrasound. If transillumination doesn’t clearly indicate a cyst, an ultrasound can help determine what else it might be. This test, which uses high-frequency sound waves to create images of structures, might be used to rule out a testicular tumor or other cause of scrotal swelling.
Treatment
Although your spermatocele probably won’t go away on its own, most spermatoceles don’t need treatment. They generally don’t cause pain or complications. If yours is painful, your doctor might recommend over-the-counter pain medications, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others).
Surgical treatment
A procedure called a spermatocelectomy generally is performed on an outpatient basis, using a local or general anesthetic. The surgeon makes an incision in the scrotum and separates the spermatocele from the epididymis.
After surgery, you might need to wear a gauze-filled athletic supporter to apply pressure to and protect the site of the incision. Your doctor might also tell you to:
- Apply ice packs for two or three days to keep swelling down
- Take oral pain medications for a day or two
- Return for a follow-up exam between one and three weeks after surgery
Possible complications from surgical removal that might affect fertility include damage to the epididymis or to the tube that transports sperm (vas deferens). It’s also possible that a spermatocele might come back, even after surgery.
Aspiration, with or without sclerotherapy
Other treatments include aspiration and sclerotherapy, though these are rarely used. During aspiration, a special needle is inserted into the spermatocele and fluid is removed (aspirated).
If the spermatocele recurs, your doctor might recommend aspirating the fluid again and then injecting an irritating chemical into the sac (sclerotherapy). The irritating agent causes the spermatocele sac to scar, which takes up the space the fluid occupied and lowers the risk of the spermatocele coming back.
Damage to the epididymis is a possible complication of sclerotherapy. It’s also possible that your spermatocele might come back.
Protecting your fertility
Surgery can potentially cause damage to the epididymis or the vas deferens, and sclerotherapy might damage the epididymis, which can affect fertility. Because of this concern, these procedures might be delayed until you’re done having children. If the spermatocele is causing so much discomfort that you don’t want to wait, talk with your doctor about the risks and benefits of sperm banking.
Preparing for your appointment
You’re likely to start by first seeing your family doctor or a general practitioner. However, you might then be referred to a doctor who specializes in treating the urinary tract and sex organs in men (urologist).
Because appointments can be brief, and there’s often a lot to remember, it’s a good idea to arrive well-prepared. Here’s some information to help you get ready for your appointment and know what to expect from your doctor.
What you can do
- Write down any symptoms you’re experiencing, including any that might seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any testicular injuries.
- Write down questions to ask your doctor.
Your time with your doctor is often limited, so preparing a list of questions can help you make the most of your time together. For spermatocele, some basic questions to ask your doctor include:
- What’s the most likely cause of my symptoms?
- What kinds of tests do I need? Do these tests require any special preparation?
- Is this condition temporary or long lasting?
- Will spermatocele affect my ability to have sex?
- Will this condition affect my fertility?
- Do I need treatment?
- What treatments are available, and which do you recommend?
- What types of side effects can I expect from treatment?
- How long after surgery do I need to wait before returning to normal activities?
- How long after surgery do I need to wait before resuming sexual activity?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
In addition to the questions that you’ve prepared to ask your doctor, don’t hesitate to ask additional questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them might reserve time to go over any points you want to spend more time on. Your doctor might ask:
- What types of symptoms are you experiencing?
- How often are you having symptoms?
- How long ago did your symptoms begin?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you experienced any trauma to your scrotal area?
What you can do in the meantime
If the spermatocele is causing pain, most people can safely take over-the-counter pain medications, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others), to ease the discomfort.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



