Rhinoplasty
![]() November, 20th, 2024
November, 20th, 2024
Summary
Learn about the benefits, risks and what to expect during nose surgery.
Overview
, Overview, ,
Rhinoplasty (RIE-no-plas-tee) is surgery that changes the shape of the nose. The reason for rhinoplasty may be to change the appearance of the nose, improve breathing or both.
The upper part of the structure of the nose is bone. The lower part is cartilage. Rhinoplasty can change bone, cartilage, skin or all three. Talk with your surgeon about whether rhinoplasty is appropriate for you and what it can achieve.
Your other facial features, the skin on your nose and what you would like to change are considered when planning the procedure. If you’re a candidate for rhinoplasty, the surgeon will develop a personal plan for you.
Sometimes part or all of a rhinoplasty is covered by insurance.
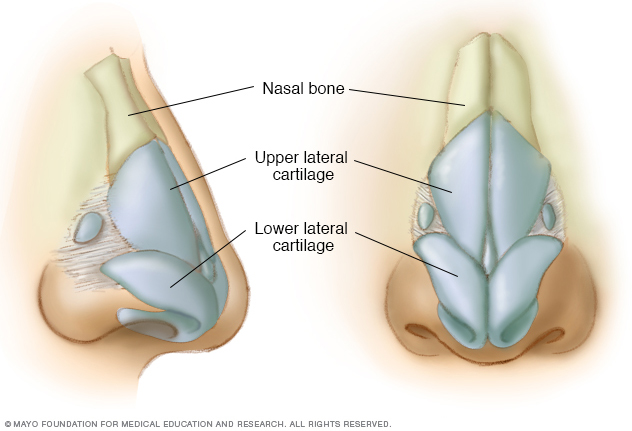
Your nose is supported by bone (at the back and bridge) and by cartilage (in the front).

At left, a woman’s nose before rhinoplasty. On the right, the same woman pictured one year after the surgery.
Rhinoplasty results Why it’s done
Rhinoplasty can change the size, shape or proportions of the nose. It may be done to fix issues from an injury, correct a birth defect or improve some breathing problems.
Risks
As with any major surgery, rhinoplasty carries risks such as:
- Bleeding.
- Infection.
- A bad reaction to the anesthesia.
Other possible risks specific to rhinoplasty include but are not limited to:
- Problems breathing through the nose.
- Permanent numbness in and around the nose.
- The possibility of an uneven-looking nose.
- Pain, discoloration or swelling that may last.
- Scarring.
- A hole in the wall between the left and right nostrils. This condition is called septal perforation.
- A need for additional surgery.
- Change in the sense of smell.
Talk to your health care provider about how these risks apply to you.
How you prepare
Before scheduling rhinoplasty, you meet with a surgeon. You talk about things that determine whether the surgery will work well for you. This meeting usually includes:
- Your medical history. The most important question is about why you want the surgery and your goals. You also answer questions about your medical history. This includes a history of nasal blockages, surgeries and any medicines you take. If you have a bleeding disorder, such as hemophilia, you may not be a candidate for rhinoplasty.
-
A physical exam. Your health care provider does a physical examination. Your facial features and the inside and outside of your nose are looked at.
The physical exam helps determine what changes need to be made. It also shows how your physical features, such as the thickness of your skin or the strength of the cartilage at the end of your nose, may affect your results. The physical exam is also important for determining how rhinoplasty will affect your breathing.
- Photographs. Photographs of your nose are taken from different angles. The surgeon may use computer software to change the photos to show you what kinds of results are possible. These photos are used for before-and-after views and reference during surgery. Most importantly, the photos let you have a specific discussion about the goals of surgery.
-
A discussion of your expectations. Talk about your reasons for surgery and what you expect. The surgeon can review with you what rhinoplasty can and can’t do for you and what your results might be. It’s normal to feel self-conscious talking about your appearance. But it’s important that you’re open with the surgeon about your desires and goals for surgery.
Looking at the overall proportions of the face and profile is important before having rhinoplasty. If you have a small chin, the surgeon may speak with you about surgery to build up your chin. This is because a small chin can create the illusion of a larger nose. It’s not required to have chin surgery, but it may better balance your facial profile.
Once the surgery is scheduled, find someone to drive you home after the procedure if you’re having an outpatient surgery.
For the first few days after anesthesia, you may forget things, have a slower reaction time and impaired judgment. Find a family member or friend to stay with you a night or two to help with personal care as you recover from surgery.
Food and medications
Don’t take medicines that have aspirin or ibuprofen (Advil, Motrin IB, others) for two weeks before and two weeks after surgery. These medicines may make you bleed more. Take only the medicines approved or prescribed by your surgeon. Avoid herbal remedies and over-the-counter supplements.
If you smoke or vape, stop. Smoking and vaping can slow healing after surgery and can result in tissue death. You could also get an infection.
What you can expect
Each rhinoplasty is customized for the person’s specific anatomy and goals.
During the procedure
You’re given medicine to put you into a sleep-like state for the surgery. This is called anesthesia. The kind of anesthesia you get depends on how complex your surgery is and what the surgeon prefers. Ask your surgeon which type of medicine is most appropriate for you.
- Local anesthesia with sedation. This type of anesthesia is usually used in an outpatient setting. It’s limited to a specific area of your body. A pain-numbing medication is injected into the nasal tissues, then you are given medicine through an intravenous (IV) line, which is a small tube placed in a vein in the hand, neck or chest. This medicine makes you groggy but not fully asleep.
- General anesthesia. You receive medicine, called anesthetic, by breathing it in or through an IV line. General anesthesia affects your entire body and causes you to be asleep during surgery. General anesthesia requires a breathing tube.
Rhinoplasty may be done inside the nose or through a small external cut, known as an incision, at the base of the nose, between the nostrils. The surgeon will likely readjust the bone and cartilage underneath the skin.
The shape of the bones or cartilage in your nose can be changed in several ways. It depends on how much needs to be taken out or added, the nose’s structure and available materials. For small changes, cartilage may be taken from deeper inside the nose or from the ear.
For larger changes, cartilage from a rib, implants or bone from other parts of the body can be used. After these changes are made, the skin on the nose and tissue are put back, and the cuts are sewn together.
Sometimes, the wall between the two sides of the nose, known as the septum, is bent or crooked. This is called a deviated septum. It can be straightened during surgery to make breathing easier.
After the surgery, you’re in a recovery room. You’re watched while you wake up. You might leave later that day or, if you have other health issues, you might stay overnight.
After the procedure
After the surgery, you need to rest in bed with your head raised higher than your chest. This reduces bleeding and swelling. Your nose may be stuffed up because of swelling. It could also be from the splints put inside your nose during surgery.
Most of the time, the internal bandages stay in place for 1 to 7 days after surgery. A splint may be taped to your nose for protection and support. It’s usually in place for about one week.
You may have a little bleeding and drainage of mucus and old blood for a few days after the surgery or after removing the dressing. A drip pad — a small piece of gauze held in place with tape — may be put under your nose to absorb drainage. Change the gauze as directed by your health care provider. Don’t put the drip pad tight against your nose.
You may be given other instructions to further lower the chances of bleeding and swelling. These should be followed for several weeks after surgery:
- Avoid intense physical activities such as aerobics and jogging.
- Take baths instead of showers while you have bandages on your nose.
- Don’t blow your nose.
- Sneeze and cough with your mouth open.
- Avoid certain facial expressions, such as smiling or laughing.
- Eat high-fiber foods, such as fruits and vegetables, to keep from getting constipated. Constipation can cause you to push hard, putting pressure on the surgery site.
- Brush your teeth gently to keep your upper lip from moving.
- Wear clothes that fasten in the front. Don’t pull clothing, such as shirts or sweaters, over your head.
In addition, don’t rest eyeglasses or sunglasses on your nose for at least four weeks after the surgery. They can put pressure on your nose. You can use cheek rests or tape the glasses to your forehead until your nose has healed.
Use SPF 30 sunscreen when you’re outside, especially on your nose. Too much sun may cause permanent discoloration on the skin of the nose.
You may have some short-term swelling or black-and-blue coloration of your eyelids 2 to 3 weeks after the surgery. Swelling of the nose can last longer, sometimes up to a year. Eating less sodium will help the swelling go away faster. Don’t put anything such as ice or cold packs on your nose after surgery.
Your nose changes throughout your life whether you have surgery or not. For this reason, it’s hard to say when you have reached your final result from the surgery. However, most of the swelling is gone within a year.
Results
Very small changes to your nose’s structure — even just a few millimeters — can make a big difference in how your nose looks. Most of the time, an experienced surgeon can get results both of you are satisfied with. But in some cases, the slight changes aren’t enough. You and your surgeon might decide to do a second surgery to make more changes. If this is the case, you must wait at least a year for the follow-up surgery because your nose can go through changes during this time.
Risks
Are there risks?
All surgeries have risks. Fortunately, rhinoplasty risks are small and complications are rare. Your health care provider talks to you about the risks and benefits before the operation.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



