Hip replacement
![]() March, 4th, 2025
March, 4th, 2025
Summary
Find out is this surgery may be an option if hip pain interferes with daily activities and nonsurgical treatments haven’t helped.
Overview
, Overview, ,
Hip replacement is surgery to remove damaged sections of the hip joint and replace them. Replacement parts are usually made of metal, ceramic and hard plastic. This artificial joint, called a prosthesis, helps reduce pain and improve function.
Hip replacement also is called total hip arthroplasty. Hip replacement might be an option if hip pain interferes with daily activities and nonsurgical treatments haven’t helped or are no longer effective. Arthritis damage is the most common reason to need hip replacement.
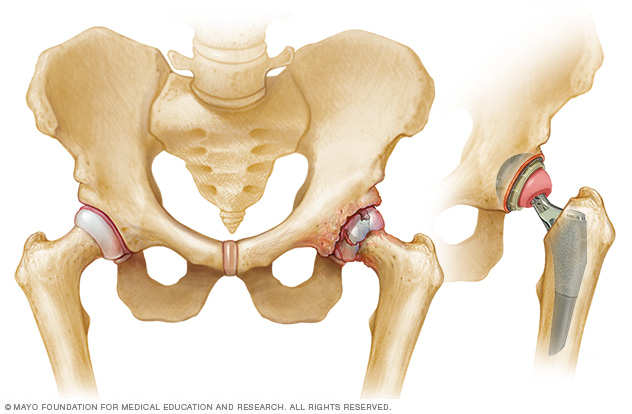
Hip prostheses are designed to mimic the ball-and-socket action of the hip joint. During hip replacement, a surgeon removes the diseased or damaged parts of the hip joint and inserts the artificial joint.
Artificial hip Why it’s done
Conditions that can damage the hip joint, sometimes making hip replacement necessary, include:
- Osteoarthritis. Commonly known as wear-and-tear arthritis, osteoarthritis damages the slick cartilage that covers the ends of bones and helps joints move smoothly.
- Rheumatoid arthritis. Caused by an overactive immune system, rheumatoid arthritis produces a type of inflammation that can erode cartilage and occasionally underlying bone. This can result in a joint that is damaged or changes shape.
- Osteonecrosis. If there isn’t enough blood supplied to the ball portion of the hip joint, the bone might collapse and change shape. Osteonecrosis might result from a dislocation or fracture that disrupts the blood supply to the bone.
Hip replacement may be an option if hip pain:
- Doesn’t stop despite taking pain medicines.
- Worsens with walking, even with a cane or walker.
- Interferes with sleep.
- Affects the ability to walk up or down stairs.
- Makes it difficult to rise from a seated position.
Risks
Risks associated with hip replacement can include:
- Blood clots. Clots can form in the leg veins after surgery. This can be dangerous because a piece of a clot can break off and travel to the lung, heart or, rarely, the brain. Blood-thinning medicines can reduce this risk.
- Infection. Infections can occur at the site of the incision and in the deeper tissue near the new hip. Most infections are treated with antibiotics. But a major infection near the new hip might require surgery to remove and replace the artificial parts.
- Fracture. During surgery, healthy portions of the hip joint might fracture. Sometimes the fractures are small enough to heal on their own. Larger fractures might need to be stabilized with wires, screws, and possibly a metal plate or bone grafts.
- Dislocation. Certain positions can cause the ball of the new joint to come out of the socket, particularly in the first few months after surgery. If the hip dislocates, a brace can help keep the hip in the correct position. If the hip keeps dislocating, surgery may be needed to stabilize it.
- Change in leg length. Surgeons take steps to avoid this problem, but occasionally a new hip makes one leg longer or shorter than the other. Sometimes this is caused by a contracture of muscles around the hip. When this happens, strengthening and stretching those muscles over time might help. Small differences in leg length usually aren’t noticeable after a few months.
- Loosening. Although this complication is rare with newer implants, the replacement joint might not become solidly fixed to the bone or might loosen over time. This can cause pain in the hip. Surgery might be needed to fix the problem.
- Nerve damage. Rarely, nerves in the area where the implant is placed can be injured. Nerve damage can cause numbness, weakness and pain.
Need for second hip replacement
Artificial hip parts might wear out eventually, especially for people who have hip replacement surgery when they’re relatively young and active. If this happens, you might need a second hip replacement. However, new materials are making implants last longer.
How you prepare
Before the operation, you’ll likely have an exam with the orthopedic surgeon. The surgeon may:
- Ask about your medical history and current medicines.
- Examine your hip, paying attention to the range of motion in your joint and the strength of the surrounding muscles.
- Order blood tests and an X-ray. An MRI is rarely needed.
During this appointment, ask any questions you have about the procedure. Be sure to find out which medicines you should avoid or continue to take in the week before surgery.
Because smoking can interfere with healing, it’s best to stop using nicotine products, including vaping, before surgery. If you need help quitting, talk with your healthcare professional.
What you can expect
When you check in for your surgery, you’re asked to remove your clothes and put on a hospital gown. You’re given either a spinal block, which numbs the lower half of your body, or a general anesthetic, which puts you into a sleeplike state.
Your surgeon might also inject a numbing medicine around nerves or in and around the joint to help block pain after your surgery.
During the procedure
The surgical procedure can usually be completed within two hours. To perform a hip replacement, the surgeon:
- Makes an incision over the hip, through the layers of tissue.
- Removes diseased and damaged bone and cartilage, leaving healthy bone intact.
- Puts the replacement socket into the pelvic bone.
- Inserts a metal stem into the top of the thighbone, which is then topped with a replacement ball.
After the procedure
After surgery, you are moved to a recovery area for a few hours while the anesthetic wears off. Medical staff monitor your blood pressure, pulse, alertness, pain or comfort level, and need for medicines.
You’re asked to breathe deeply, cough or blow into a device to help keep fluid out of your lungs. How long you stay after surgery depends on your individual needs. Many people can go home that same day.
Blood clot prevention
After hip replacement, you’re at increased risk of blood clots in your legs for a short time. Possible measures to prevent this complication include:
- Moving early. You’re encouraged to sit up and walk with crutches or a walker soon after surgery.
- Applying pressure. Both during and after surgery, you might wear elastic compression stockings or inflatable air sleeves on your lower legs. The air sleeves squeeze and release your legs. That helps keep blood from pooling in the leg veins, reducing the chance that clots will form.
- Taking blood-thinning medicines. Your surgeon might prescribe a blood thinner that you take as a shot or by mouth after surgery. Depending on how soon you walk, how active you are and your overall risk of blood clots, you might need blood thinners for several weeks after surgery.
Physical therapy
Daily activity and exercise can help you regain the use of your joint and muscles. A physical therapist can recommend strengthening and mobility exercises. The therapist also can help you learn how to use a walking aid, such as a walker, a cane or crutches. As therapy goes on, you slowly increase the amount of weight you put on your leg until you’re able to walk without assistance.
Home recovery
Before you leave the hospital, you and your caregivers get tips on caring for your new hip. For a smooth transition:
- Arrange to have a friend or relative prepare some meals in advance.
- Place everyday items at waist level so you won’t have to bend down or reach up.
- Consider getting a raised toilet seat and a shower chair for your recovery at home.
- Put your phone, tissues, TV remote, medicine and books near the area where you’ll be spending most of your time during recovery.
Results
Full recovery from a hip replacement varies from person to person, but most people are doing well three months after the surgery. Improvements typically continue during the first year after surgery.
The new hip joint can reduce pain and increase the hip’s range of motion. But don’t expect to do everything you could do before the hip became painful.
High-impact activities, such as running or playing basketball, might be too stressful on the artificial joint. But in time, most people can participate in lower impact activities — such as swimming, golfing and bicycle riding.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



